Abstract
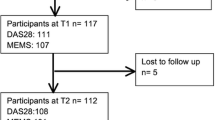
Polypharmacy can be associated with poor outcomes in chronic diseases. Our objective is to determine the prevalence of polypharmacy and its association with disease control in patients with rheumatoid arthritis (RA) and systemic lupus erythematosus (SLE). An observational study was conducted using the SARD database of the CHU de Québec. Participants newly diagnosed with RA or SLE enrolled in the database after 24 months were included. Collected data included number and type of medications, Charlson Comorbidity Index, and medication adherence (proportion of days covered during the first 180 days). Polypharmacy was defined as the simultaneous use ≥5 medications. Multivariable logistic and linear regressions were used to determine the association between polypharmacy and disease control (DAS28CRP, SLEDAI-2 K). The study included 111 participants (RA = 81; SLE = 30). Medication count increased at two years in RA (mean ± SD): 4.6 ± 3.3 to 6.9 ± 3.6; and SLE: 6.5 ± 4.6 to 7.80 ± 4.82. Polypharmacy prevalence increased at two years: RA: from 43 to 74%; SLE: from 47 to 73%. Mean medication adherence exceeded 85%. For RA participants, polypharmacy was associated with a better DAS28CRP score at one year [adjusted odds ratio of achieving a poor outcome: 0.17 (95%CI 0.04–0.71)], but this association was lost at two years [2.88 (0.45–18.29)]. For SLE, polypharmacy was not associated with disease activity based on the SLEDAI-2 K at one year [7.36 (0.26-211.16)] or two years [0.32 (0.05–1.99)]. Overall, polypharmacy is very prevalent in RA and SLE and could be positively associated with the level of disease control in the year after a diagnosis of RA.
Similar content being viewed by others
Data availability
The data underlying this article will be shared on reasonable request to the corresponding author.
References
Delara M, Murray L, Jafari B, Bahji A, Goodarzi Z, Kirkham J, Chowdhury Z, Seitz D (2022) Prevalence and factors associated with polypharmacy: a systematic review and meta-analysis. BMC Geriatr 22:601. https://doi.org/10.1186/s12877-022-03279-x
Masnoon N, Shakib S, Kalisch-Ellett L, Caughey GE (2017) What is polypharmacy? A systematic review of definitions. BMC Geriatr 17:230. https://doi.org/10.1186/s12877-017-0621-2
Gosselin E, Simard M, Dubé M, Sirois C (2020) Portrait de la polypharmacie chez les aînés québécois entre 2000 et 2016. Institut national de santé publique du Québec, Québec; Gouvernement du Québec. https://www.inspq.qc.ca/sites/default/files/publications/2679_portrait_polypharmacie_aines_quebecois.pdf
Rodrigues MC, Oliveira CD (2016) Drug-drug interactions and adverse drug reactions in polypharmacy among older adults: an integrative review. Rev Lat Am Enfermagem 24:e2800. https://doi.org/10.1590/1518-8345.1316.2800
Miller GE, Sarpong EM, Davidoff AJ, Yang EY, Brandt NJ, Fick DM (2017) Determinants of potentially inappropriate medication use among community-dwelling older adults. Health Serv Res 52(4):1534–1549. https://doi.org/10.1111/1475-6773.12562
Wallace E, Stuart E, Vaughan N, Bennett K, Fahey T, Smith SM (2014) Risk prediction models to predict emergency hospital admission in community-dwelling adults. Med Care 52(8):751–765. https://doi.org/10.1097/MLR.0000000000000171
Leelakanok N, Holcombe AL, Bund BC, Gu X, Schweizer ML (2017) Association between polypharmacy and death: a systematic review and meta-analysis. J Am Pharm Assoc 57(6):729–738. https://doi.org/10.1016/j.japh.2017.06.002
Ziade N, El Khoury B, Zoghbi M, Merheb G, Abi Karam G, Mroue’ K, Messaykeh J (2020) Prevalence and pattern of comorbidities in chronic rheumatic and musculoskeletal diseases: the COMORD study. Sci Rep 10(1):7683. https://doi.org/10.1038/s41598-020-64732-8
Jack JD, McCutchan R, Maier S, Schirmer M (2020) Polypharmacy in Middle-European rheumatoid arthritis-patients: a retrospective longitudinal cohort analysis with systematic literature review. Front Med 7:573542. https://doi.org/10.3389/fmed.2020.573542
Bechman K, Clarke BD, Rutherford AI, Yates M, Nikiphorou E, Molokhia M, Norton S, Cope AP, Hyrich KL, Galloway JB (2019) Polypharmacy is associated with treatment response and serious adverse events: results from the British society for rheumatology biologics register for rheumatoid arthritis. Rheumatology 58(10):1767–1776. https://doi.org/10.1093/rheumatology/kez037
Filkova M, Carvalho J, Norton S, Scott D, Mant T, Molokhia M, Cope A, Galloway J (2017) Polypharmacy and unplanned hospitalizations in patients with rheumatoid arthritis. J Rheumatol 44(12):1786–1793. https://doi.org/10.3899/jrheum.160818
Lourenço MD, Carli FV, De Assis MR (2018) Characterization of falls in adults with established rheumatoid arthritis and associated factors. Adv Rheumatol 58(1):16. https://doi.org/10.1186/s42358-018-0021-0
Oh K, Furuya T, Ikari K, Inoue E, Tanaka E, Yamanaka H, Okazaki K, Harigai M (2021) Polypharmacy, declined walking speed, bent back, and disability associated with a history of falls in Japanese patients with rheumatoid arthritis: results from the IORRA cohort study. Mod Rheumatol 31(3):764–767. https://doi.org/10.1080/14397595.2020.1812200
González-Gamboa LM, Barocio-Ramírez AK, Rocha-Muñoz AD, De Santos-Ávila F, Meda-Lara RM, González-López L, Gámez-Nava JI, Gómez-Bañuelos E, Chavarria-Avila E, Durán-Barragán S, Navarro-Hernández RE, Pizano-Martínez OE, Nuñez-Atahualpa L, del Vázquez- M (2016) Disease activity score on 28 joints and polypharmacy are independent predictors for health-related quality of life evaluated by INCAVISA in patients with rheumatoid arthritis. J Clin Rheumatol 22(8):399–404. https://doi.org/10.1097/RHU.0000000000000463
Séguin DJ, Peschken CA, Dolovich C, Grymonpre RE, St. John PD, Tisseverasinghe A (2023) Polypharmacy and potentially inappropriate medication use in older adults with systemic lupus erythematosus. Arthritis Care Res 75(2):356–364. https://doi.org/10.1002/acr.24766
Wells GA, Becker JC, Teng J, Dougados M, Schiff M, Smolen JS, Aletaha D, Van Riel P (2009) Validation of the 28-joint disease activity score (DAS28) and European League against Rheumatism response criteria based on C-reactive protein against disease progression in patients with rheumatoid arthritis, and comparison with the DAS28 based on erythrocyte sedimentation rate. Ann Rheum Dis 68(6):954–960. https://doi.org/10.1136/ard.2007.084459
Aletaha D, Nell V, Stamm T, Uffmann M, Pflugbeil S, Machold K, Smolen JS (2005) Acute phase reactants add little to composite disease activity indices for rheumatoid arthritis: validation of a clinical activity score. Arthritis Res Ther 7(4):R796–806. https://doi.org/10.1186/ar1740
Gladman DD, Ibañez D, Urowitz MB (2002) Systemic lupus erythematosus disease activity index 2000. J Rheumatol 29(2):288–291
Yazdany J, Yelin EH, Panopalis P, Trupin L, Julián L, Katz PP (2008) Validation of the systemic lupus erythematosus activity questionnaire in a large observational cohort. Arthritis Rheum 59(1):136–143. https://doi.org/10.1002/art.23238
Charlson ME, Pompei P, Ales KL, MacKenzie C (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40(5):373–383. https://doi.org/10.1016/0021-9681(87)90171-8
Charlson M, Szatrowski TP, Peterson J, Gold J (1994) Validation of a combined comorbidity index. J Clin Epidemiol 47(11):1245–1251. https://doi.org/10.1016/0895-4356(94)90129-5
Prieto-Merino D, Mulick A, Armstrong C, Hoult H, Fawcett S, Eliasson L, Clifford S (2021) Estimating proportion of days covered (PDC) using real-world online medicine suppliers’ datasets. J Pharm Policy Pract 14(1):113. https://doi.org/10.1186/s40545-021-00385-w
Coskun Benlidayi I (2019) Polypharmacy in geriatric rheumatology. Rheumatol Int 39(6):1115–1116. https://doi.org/10.1007/s00296-019-04264-1
Miyake H, Sada RM, Akebo H, Tsugihashi Y, Hatta K (2023) Prevalence and factors associated with polypharmacy among patients with rheumatoid arthritis: a single-centre, cross-sectional study. Clin Rheumatol 42(9):2287–2295. https://doi.org/10.1007/s10067-023-06646-0
Khader Y, Beran A, Ghazaleh S, Lee-Smith W, Altorok N (2022) Predictors of remission in rheumatoid arthritis patients treated with biologics: a systematic review and meta-analysis. Clin Rheumatol 41(12):3615–3627. https://doi.org/10.1007/s10067-022-06307-8
Ranganath VK, Maranian P, Elashoff D, Woodworth T, Khanna D, Hahn TJ, Sarkisian CA, Kremer JM, Fürst DE, Paulus HE (2013) Comorbidities are associated with poorer outcomes in community patients with rheumatoid arthritis. Rheumatology 52(10):1809–1817. https://doi.org/10.1093/rheumatology/ket224
Yoshii I, Sawada N, Chijiwa T (2022) Clinical characteristics and variants that predict prognosis of difficult-to-treat rheumatoid arthritis. Rheumatol Int 42(11):1947–1954. https://doi.org/10.1007/s00296-022-05124-1
Takanashi S, Kaneko Y, Takeuchi T (2021) Characteristics of patients with difficult-to-treat rheumatoid arthritis in clinical practice. Rheumatology 60(11):5247–5256. https://doi.org/10.1093/rheumatology/keab209
Arnaud L, Tektonidou MG (2020) Long-term outcomes in systemic lupus erythematosus: trends over time and major contributors. Rheumatology 59(Suppl5):v29–v38. https://doi.org/10.1093/rheumatology/keaa382
Désiré Diendéré RJ, Jean S, Sirois C (2021) La polypharmacie chez les adultes québécois de moins de 65 ans assurés par le régime public d’assurance médicaments du Québec (RPAM): description et analyse. Master’s thesis, Université Laval
Kara M, Alp G, Palanbek Yavaş S, Taşdemir A, Ketenci S, Kara MM, Ozduran E (2023) The effect of polypharmacy on rheumatoid and psoriatic arthritis treatment: retrospective study. PeerJ 11:e16418. https://doi.org/10.7717/peerj.16418
Kim GJ, Lee JS, Jang S, Lee S, Jeon S, Lee S, Kim JH, Lee KH (2024) Polypharmacy and elevated risk of severe adverse events in older adults based on the Korea Institute of drug safety and risk management-korea adverse event reporting system database. J Korean Med Sci 39(28):e205. https://doi.org/10.3346/jkms.2024.39.e205
Campeau Calfat A, Turner JP, Simard M, Boiteau V, Sirois C (2024) Association between number of medications and indicators of potentially inappropriate polypharmacy: a population-based cohort of older adults in Quebec, Canada. Ther Adv Drug Saf 15:1–17. https://doi.org/10.1177/20420986241309882
Davies LE, Spiers G, Kingston A, Todd A, Adamson J, Hanratty B (2020) Adverse outcomes of polypharmacy in older people: systematic review of reviews. J Am Med Dir Assoc 21(2):181–187. https://doi.org/10.1016/j.jamda.2019.10.022
Toh JJ, Zhang H, Soh YY, Zhang Z, Wu XV (2023) Prevalence and health outcomes of polypharmacy and hyperpolypharmacy in older adults with frailty: a systematic review and meta-analysis. Ageing Res Rev 83:101811. https://doi.org/10.1016/j.arr.2022.101811
Fraenkel L, Bathon JM, England BR, St Clair EW, Arayssi T, Carandang K, Deane KD, Genovese MC, Huston K, Kerr GS, Kremer JM, Nakamura MC, Russell L, Singh JA, Smith BJ, Sparks JA, Venkatachalam S, Weinblatt ME, Al-Gibbawi M, Akl EA et al (2021) 2021 American College of Rheumatology Guideline for the treatment of rheumatoid arthritis. Arthritis Care Res 73(7):924–939. https://doi.org/10.1002/acr.24596
Smolen JS, Landewé R, Bergstra SA, Kerschbaumer A, Sepriano A, Aletaha D, Caporali R, Edwards CJ, Hyrich KL, Pope J, De Souza S, Stamm T, Takeuchi T, Verschueren P, Winthrop K, Balsa A, Bathon JM, Buch MH, Burmester GR, Van Der Heijde D et al (2022) EULAR recommendations for the management of rheumatoid arthritis with synthetic and biological disease-modifying antirheumatic drugs: 2022 update. Ann Rheum Dis 82(1):3–18. https://doi.org/10.1136/ard-2022-223356
Fanouriakis A, Kostopoulou M, Alunno A, Aringer M, Bajema IM, Boletis J, Cervera R, Doria A, Gordon C, Govoni M, Houssiau F, Jayne D, Kouloumas M, Kuhn A, Larsen JL, Lerstrøm K, Moroni G, Mosca M, Schneider M, Boumpas DT et al (2019) 2019 update of the EULAR recommendations for the management of systemic lupus erythematosus. Ann Rheum Dis 78(6):736–745. https://doi.org/10.1136/annrheumdis-2019-215089
Van Den Bemt BJF, Zwikker H, Van Den Ende C (2012) Medication adherence in patients with rheumatoid arthritis: a critical appraisal of the existing literature. Expert Rev Clin Immunol 8(4):337–351. https://doi.org/10.1586/eci.12.23
Costedoat-Chalumeau N, Pouchot J, Guettrot-Imbert G, Guern VL, Leroux G, Marra D, Morel N, Piette J (2013) Adherence to treatment in systemic lupus erythematosus patients. Best Pract Res Clin Rheumatol 27(3):329–340. https://doi.org/10.1016/j.berh.2013.07.001
Hardy C, Gladman DD, Su J, Rozenbojm N, Urowitz MB (2021) Barriers to medication adherence and degree of nonadherence in a systemic lupus erythematosus (SLE) outpatient population. Rheumatol Int 41(8):1457–1464. https://doi.org/10.1007/s00296-021-04898-0
Wong PK (2016) Medication adherence in patients with rheumatoid arthritis: why do patients not take what we prescribe? Rheumatol Int 36(11):1535–1542. https://doi.org/10.1007/s00296-016-3566-4
Rintelen B, Sautner J, Haindl P, Andel I, Maktari A, Leeb B (2009) Comparison of three rheumatoid arthritis disease activity scores in clinical routine. Scand J Rheumatol 38(5):336–341. https://doi.org/10.1080/03009740902932835
Miyake H, Sada RM, Akebo H, Tsugihashi Y, Hatta K (2023) Polypharmacy prevalence and associated factors in patients with systemic lupus erythematosus: a single-centre, cross-sectional study. Mod Rheumatol 34(1):106–112. https://doi.org/10.1093/mr/roac155
Acknowledgements
Dr. Paul R. Fortin is supported by a Tier 1 Canada Research Chair on Systemic Autoimmune Rheumatic Diseases. Caroline Sirois was recipient of Junior 2 Research Scholar from the Fonds de Recherche du Québec – Santé (FRQS).
Funding
The SARD biobank and database (SARD BDB) of the CHU de Québec-Université Laval is supported by the Fondation du CHU de Québec-Université Laval.
Author information
Authors and Affiliations
Contributions
All authors take full responsibility for the integrity and accuracy of all aspects of the work.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest.
Use of artificial intelligence
This article was written without the use of artificial intelligence and has not been reviewed by a commercial editing service.
Congress abstract publication
An earlier version of the abstract before final analysis was presented at the Canadian Rheumatology Association 2023 Annual Scientific Meeting: Berthelot W, Sirois C, Julien AS, Amiable N, Fortin PR (2023) Polypharmacy in Systemic Autoimmune Rheumatic Diseases. Canadian Rheumatology Association Meeting Quebec City Convention Centre Quebec City, Quebec, Canada February 8–11, 2023. J Rheumatol 50(7 Suppl 1):7-100. https://doi.org/10.3899/jrheum.2023-0216.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Berthelot, W., Sirois, C., Julien, AS. et al. The association between polypharmacy and disease control in rheumatoid arthritis and systemic lupus erythematosus: a cohort study. Rheumatol Int 45, 44 (2025). https://doi.org/10.1007/s00296-025-05804-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00296-025-05804-8