Abstract
Uveitis encompasses multiple different conditions that are all characterized by intra-ocular inflammation. Uveitis occurs in the context of many different rheumatological conditions and carries a substantial risk to vision. Uveitis can develop both at the early stages of rheumatic diseases, sometimes even preceding other clinical features, and at later stages of disease. Uveitis can also occur as either a direct or an indirect complication of therapies used to treat patients with rheumatic disease. Conversely, patients with uveitis of non-rheumatic aetiology sometimes require immunosuppression, a treatment option that is not readily accessible to ophthalmologists. Thus, collaborative working between rheumatologists and ophthalmologists is critical for optimal management of patients with uveitis. This Review is written with rheumatologists in mind, to assist in the care of patients with uveitis. We collate and summarize the latest evidence and best practice in the diagnosis, management and prognostication of uveitis, including future trends and research priorities.
Key points
-
Uveitis accounts for up to 10% of visual impairment globally, highlighting the need for prompt recognition and management.
-
TNF inhibitors have significantly improved outcomes in both adult and paediatric uveitis, with the strongest evidence for adalimumab. An exception is etanercept, which worsens uveitis.
-
The second-line biologic option for uveitis is IL-6 inhibitors, with intravenous tocilizumab having the most substantial supporting evidence.
-
Collaborative work between rheumatologists and ophthalmologists is critical for optimal management of uveitis.
-
More trials are needed in uveitis, as there is a wide array of novel molecules available for systemic rheumatic diseases that should be explored for therapeutic use in uveitis.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Jabs, D. A. & Busingye, J. Approach to the diagnosis of the uveitides. Am. J. Ophthalmol. 156, 228–236 (2013).
Jabs, D. A. Epidemiology of uveitis. Ophthalmic Epidemiol. 15, 283–284 (2008).
Miserocchi, E., Fogliato, G., Modorati, G. & Bandello, F. Review on the worldwide epidemiology of uveitis. Eur. J. Ophthalmol. 23, 705–717 (2013).
Jabs, D. A., Nussenblatt, R. B., Rosenbaum, J. T. & Standardization of uveitis nomenclature for reporting clinical data. Results of the First International Workshop. Am. J. Ophthalmol. 140, 509–516 (2005).
Trusko, B. et al. The Standardization of Uveitis Nomenclature (SUN) Project. Development of a clinical evidence base utilizing informatics tools and techniques. Methods Inf. Med. 52, 259–265 (2013). s251–256.
Chang, M. H., Shantha, J. G., Fondriest, J. J., Lo, M. S. & Angeles-Han, S. T. in: Rheumatic Disease Clinics of North America. 47, 619-641 (W.B. Saunders, 2021).
Sabri, K., Saurenmann, R. K., Silverman, E. D. & Levin, A. V. Course, complications, and outcome of juvenile arthritis-related uveitis. J. AAPOS 12, 539–545 (2008).
Rypdal, V. et al. Uveitis in juvenile idiopathic arthritis: 18-year outcome in the population-based Nordic cohort study. Ophthalmology 128, 598–608 (2021).
Kopplin, L. J., Mount, G. & Suhler, E. B. Review for disease of the year: epidemiology of HLA-B27 associated ocular disorders. Ocul. Immunol. Inflamm. 24, 470–475 (2016).
Abraham, A., Nicholson, L., Dick, A., Rice, C. & Atan, D. Intermediate uveitis associated with MS: diagnosis, clinical features, pathogenic mechanisms, and recommendations for management. Neurol. Neuroimmunol. Neuroinflamm. 8, e909 (2020).
Kreps, E. O. et al. Long-term visual outcome of patients with Blau syndrome. Ocul. Immunol. Inflamm. 32, 1728–1732 (2024).
Bertrand, P. J. et al. Uveitis: autoimmunity… and beyond. Autoimmun. Rev. 18, 102351 (2019).
Smith, J. R. & Rosenbaum, J. T. Management of uveitis: a rheumatologic perspective. Arthritis Rheum. 46, 309–318 (2002).
Joltikov, K. A. & Lobo-Chan, A. M. Epidemiology and risk factors in non-infectious uveitis: a systematic review. Front. Med. 8, 695904 (2021).
Maghsoudlou, P. et al. Uveitis associated with monogenic autoinflammatory syndromes in children. Ocul. Immunol. Inflamm. 31, 1930–1943 (2023).
Ramos-Casals, M. et al. Autoimmune diseases induced by TNF-targeted therapies: analysis of 233 cases. Medicine 86, 242–251 (2007).
Lim, L. L., Fraunfelder, F. W. & Rosenbaum, J. T. Do tumor necrosis factor inhibitors cause uveitis? A registry-based study. Arthritis Rheum. 56, 3248–3252 (2007).
Chartrand, N. A. et al. Ocular side effects of bisphosphonates: a review of literature. J. Ocul. Pharmacol. Ther. 39, 3–16 (2023).
Coates, L. C., McGonagle, D. G., Bennett, A. N., Emery, P. & Marzo-Ortega, H. Uveitis and tumour necrosis factor blockade in ankylosing spondylitis. Ann. Rheum. Dis. 67, 729–730 (2008).
Nicolela Susanna, F. & Pavesio, C. A review of ocular adverse events of biological anti-TNF drugs. J. Ophthalmic Inflamm. Infect. 10, 11 (2020).
Peris, P., Monegal, A. & Guanabens, N. Bisphosphonates in inflammatory rheumatic diseases. Bone 146, 115887 (2021).
Anquetil, C. et al. Evolving spectrum of drug-induced uveitis at the era of immune checkpoint inhibitors results from the WHO’s pharmacovigilance database. J. Autoimmun. 111, 102454 (2020).
Fietta, P., Manganelli, P. & Lodigiani, L. Clodronate induced uveitis. Ann. Rheum. Dis. 62, 378 (2003).
Egwuagu, C. E., Alhakeem, S. A. & Mbanefo, E. C. Uveitis: molecular pathogenesis and emerging therapies. Front. Immunol. 12, 623725 (2021).
Read, R. W. Uveitis: advances in understanding of pathogenesis and treatment. Curr. Rheumatol. Rep. 8, 260–266 (2006).
International Team for the Revision of the International Criteria for Behçet’s Disease. The International Criteria for Behçet’s Disease (ICBD): a collaborative study of 27 countries on the sensitivity and specificity of the new criteria. J. Eur. Acad. Dermatol. Venereol. 28, 338–347 (2014).
Rudwaleit, M. et al. The development of Assessment of SpondyloArthritis international Society classification criteria for axial spondyloarthritis (part I): classification of paper patients by expert opinion including uncertainty appraisal. Ann. Rheum. Dis. 68, 770–776 (2009).
Rudwaleit, M. et al. The Assessment of SpondyloArthritis International Society classification criteria for peripheral spondyloarthritis and for spondyloarthritis in general. Ann. Rheum. Dis. 70, 25–31 (2011).
Judson, M. A. et al. The WASOG sarcoidosis organ assessment instrument: an update of a previous clinical tool. Sarcoidosis Vasc. Diffus. Lung Dis. 31, 19–27 (2014).
Petty, R. E. et al. International League of Associations for Rheumatology classification of juvenile idiopathic arthritis: second revision, Edmonton, 2001. J. Rheumatol. 31, 390–392 (2004).
Fernández-Melón, J. et al. Uveitis as the initial clinical manifestation in patients with spondyloarthropathies. J. Rheumatol. 31, 524–527 (2004).
Standardization of Uveitis Nomenclature Working Group. Classification criteria for Behçet disease uveitis. Am. J. Ophthalmol. 228, 80–88 (2021).
Standardization of Uveitis Nomenclature Working Group. Classification criteria for juvenile idiopathic arthritis-associated chronic anterior uveitis. Am. J. Ophthalmol. 228, 192–197 (2021).
Standardization of Uveitis Nomenclature Working Group. Classification criteria for spondyloarthritis/HLA-B27-associated anterior uveitis. Am. J. Ophthalmol. 228, 117–125 (2021).
Standardization of Uveitis Nomenclature Working Group Classification criteria for sarcoidosis-associated uveitis. Am. J. Ophthalmol. 228, 220–230 (2021).
Mudie, L. I. et al. Evaluation of the SUN classification criteria for uveitides in an academic uveitis practice. Am. J. Ophthalmol. 241, 57–63 (2022).
Kuemmerle-Deschner, J. B. et al. Diagnostic criteria for cryopyrin-associated periodic syndrome (CAPS). Ann. Rheum. Dis. 76, 942–947 (2017).
Dick, A. D. et al. Guidance on noncorticosteroid systemic immunomodulatory therapy in noninfectious uveitis: Fundamentals Of Care for UveitiS (FOCUS) Initiative. Ophthalmology 125, 757–773 (2018).
Angeles-Han, S. T. et al. 2019 American College of Rheumatology/Arthritis Foundation Guideline for the Screening, Monitoring, and Treatment of Juvenile Idiopathic Arthritis-Associated Uveitis. Arthritis Rheumatol. 71, 864–877 (2019).
Tsirouki, T. et al. A focus on the epidemiology of uveitis. Ocul. Immunol. Inflamm. 26, 2–16 (2018).
Kothari, S. et al. The risk of intraocular pressure elevation in pediatric noninfectious uveitis. Ophthalmology 122, 1987–2001 (2015).
Thorne, J. E., Woreta, F. A., Dunn, J. P. & Jabs, D. A. Risk of cataract development among children with juvenile idiopathic arthritis-related uveitis treated with topical corticosteroids. Ophthalmology 117, 1436–1441 (2010).
Sen, H. N. et al. Periocular corticosteroid injections in uveitis: effects and complications. Ophthalmology 121, 2275–2286 (2014).
Lightman, S. et al. Vision-related functioning outcomes of dexamethasone intravitreal implant in noninfectious intermediate or posterior uveitis. Investig. Ophthalmol. Vis. Sci. 54, 4864–4870 (2013).
Lowder, C. et al. Dexamethasone intravitreal implant for noninfectious intermediate or posterior uveitis. Arch. Ophthalmol. 129, 545–553 (2011).
Jaffe, G. J. et al. Long-term follow-up results of a pilot trial of a fluocinolone acetonide implant to treat posterior uveitis. Ophthalmology 112, 1192–1198(2005).
Thorne, J. E. et al. Periocular triamcinolone vs. intravitreal triamcinolone vs. intravitreal dexamethasone implant for the treatment of uveitic macular edema: the PeriOcular vs. INTravitreal corticosteroids for uveitic macular edema (POINT) Trial. Ophthalmology 126, 283–295 (2019).
Callanan, D. G., Jaffe, G. J., Martin, D. F., Pearson, P. A. & Comstock, T. L. Treatment of posterior uveitis with a fluocinolone acetonide implant: three-year clinical trial results. Arch. Ophthalmol. 126, 1191–1201 (2008).
Multicenter Uveitis Steroid Treatment (MUST) Trial Research Group. Benefits of systemic anti-inflammatory therapy versus fluocinolone acetonide intraocular implant for intermediate uveitis, posterior uveitis, and panuveitis: fifty-four-month results of the Multicenter Uveitis Steroid Treatment (MUST) trial and follow-up study. Ophthalmology 122, 1967–1975 (2015).
Yeh, S. et al. Efficacy and safety of suprachoroidal CLS-TA for macular edema secondary to noninfectious uveitis: phase 3 randomized trial. Ophthalmology 127, 948–955 (2020).
Habot-Wilner, Z. et al. Periocular corticosteroid injection in the management of uveitis in children. Acta Ophthalmol. 88, e299–e304 (2010).
Jabs, D. A. Immunosuppression for the uveitides. Ophthalmology 125, 193–202 (2018).
Da Silva, J. A. et al. Safety of low dose glucocorticoid treatment in rheumatoid arthritis: published evidence and prospective trial data. Ann. Rheum. Dis. 65, 285–293 (2006).
Constantin, T. et al. Consensus-based recommendations for the management of uveitis associated with juvenile idiopathic arthritis: the SHARE initiative. Ann. Rheum. Dis. 77, 1107–1117 (2018).
Nguyen, Q. D. et al. A cross-sectional study of the current treatment patterns in noninfectious uveitis among specialists in the United States. Ophthalmology 118, 184–190 (2011).
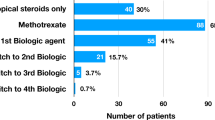
Esteban-Ortega, M. et al. An observational study in the real clinical practice of the treatment of noninfectious uveitis. J. Clin. Med. 13, 1402 (2024).
Jabs, D. A. et al. Guidelines for the use of immunosuppressive drugs in patients with ocular inflammatory disorders: recommendations of an expert panel. Am. J. Ophthalmol. 130, 492–513 (2000).
Deuter, C. M. E. et al. Enteric-coated mycophenolate sodium in the treatment of non-infectious intermediate uveitis: results of a prospective, controlled, randomised, open-label, early terminated multicentre trial. Br. J. Ophthalmol. 102, 647–653 (2018).
Yazici, H. et al. A controlled trial of azathioprine in Behçet’s syndrome. N. Engl. J. Med. 322, 281–285 (1990).
Rathinam, S. R. et al. Effect of corticosteroid-sparing treatment with mycophenolate mofetil vs methotrexate on inflammation in patients with uveitis: a randomized clinical trial. JAMA 322, 936–945, (2019).
Murphy, C. C. et al. Cyclosporine vs tacrolimus therapy for posterior and intermediate uveitis. Arch. Ophthalmol. 123, 634–641 (2005).
Kempen, J. H. et al. Methods for identifying long-term adverse effects of treatment in patients with eye diseases: the Systemic Immunosuppressive Therapy for Eye Diseases (SITE) cohort study. Ophthalmic Epidemiol. 15, 47–55 (2008).
Gangaputra, S. et al. Methotrexate for ocular inflammatory diseases. Ophthalmology 116, 2188–2198.e2181 (2009).
Daniel, E. et al. Mycophenolate mofetil for ocular inflammation. Am. J. Ophthalmol. 149, 423–432.e421-422 (2010).
Pasadhika, S. et al. Azathioprine for ocular inflammatory diseases. Am. J. Ophthalmol. 148, 500–509.e2 (2009).
Kaçmaz, R. O. et al. Cyclosporine for ocular inflammatory diseases. Ophthalmology 117, 576–584 (2010).
Benitez-Del-Castillo, J. M., Garcia-Sanchez, J., Iradier, T. & Bañares, A. Sulfasalazine in the prevention of anterior uveitis associated with ankylosing spondylitis. Eye 14, 340–343 (2000).
Muñoz-Fernández, S. et al. Sulfasalazine reduces the number of flares of acute anterior uveitis over a one-year period. J. Rheumatol. 30, 1277–1279 (2003).
Ramiro, S. et al. ASAS-EULAR recommendations for the management of axial spondyloarthritis: 2022 update. Ann. Rheum. Dis. 82, 19–34 (2023).
Knickelbein, J. E., Kim, M., Argon, E., Nussenblatt, R. B. & Sen, N. H. Comparative efficacy of steroid-sparing therapies for non-infectious uveitis. Expert Rev. Ophthalmol. 12, 313–319 (2017).
Foeldvari, I. & Wierk, A. Methotrexate is an effective treatment for chronic uveitis associated with juvenile idiopathic arthritis. J. Rheumatol. 32, 362–365 (2005).
Heiligenhaus, A., Mingels, A., Heinz, C. & Ganser, G. Methotrexate for uveitis associated with juvenile idiopathic arthritis: value and requirement for additional anti-inflammatory medication. Eur. J. Ophthalmol. 17, 743–748 (2007).
Papadopoulou, C. et al. Methotrexate therapy may prevent the onset of uveitis in juvenile idiopathic arthritis. J. Pediatr. 163, 879–884 (2013).
Shetty, A. K., Zganjar, B. E., Ellis, G. S. Jr., Ludwig, I. H. & Gedalia, A. Low-dose methotrexate in the treatment of severe juvenile rheumatoid arthritis and sarcoid iritis. J. Pediatr. Ophthalmol. Strabismus 36, 125–128 (1999).
Mackensen, F. et al. Randomized controlled study to evaluate the efficacy of adalimumab in patients with different forms of refractory uveitis. Ocul. Immunol. Inflamm. 26, 1015–1022 (2018).
Jaffe, G. J. et al. Adalimumab in patients with active noninfectious uveitis. N. Engl. J. Med. 375, 932–943 (2016).
Nguyen, Q. D. et al. Adalimumab for prevention of uveitic flare in patients with inactive non-infectious uveitis controlled by corticosteroids (VISUAL II): a multicentre, double-masked, randomised, placebo-controlled phase 3 trial. Lancet 388, 1183–1192 (2016).
Suhler, E. B. et al. Safety and efficacy of adalimumab in patients with noninfectious uveitis in an ongoing open-label study: VISUAL III. Ophthalmology 125, 1075–1087 (2018).
Rudwaleit, M. et al. Adalimumab effectively reduces the rate of anterior uveitis flares in patients with active ankylosing spondylitis: results of a prospective open-label study. Ann. Rheum. Dis. 68, 696–701 (2009).
García-Beloso, N. et al. Switching between reference adalimumab and biosimilars in chronic immune-mediated inflammatory diseases: a systematic literature review. Br. J. Clin. Pharmacol. 88, 1529–1550 (2022).
Song, S. H. & Woo, S. J. Efficacy and safety of switching from adalimumab originator to SB5, adalimumab biosimilar for noninfectious uveitis. Ocul. Immunol. Inflamm. 32, 1755–1759 (2024).
Suhler, E. B. et al. A prospective trial of infliximab therapy for refractory uveitis: preliminary safety and efficacy outcomes. Arch. Ophthalmol. 123, 903–912, (2005).
Kruh, J. N., Yang, P., Suelves, A. M. & Foster, C. S. Infliximab for the treatment of refractory noninfectious uveitis: a study of 88 patients with long-term follow-up. Ophthalmology 121, 358–364 (2014).
Takeuchi, M. et al. Ten-year follow-up of infliximab treatment for uveitis in Behçet disease patients: a multicenter retrospective study. Front. Med. 10, 1095423 (2023).
Giardina, A. et al. One year study of efficacy and safety of infliximab in the treatment of patients with ocular and neurological Behçet’s disease refractory to standard immunosuppressive drugs. Rheumatol. Int. 31, 33–37 (2011).
Calvo-Río, V. et al. Golimumab in refractory uveitis related to spondyloarthritis. Multicenter study of 15 patients. Semin. Arthritis Rheum. 46, 95–101 (2016).
Okada, K., Zhou, Y., Hashida, N., Takagi, T. & Tian, Y. S. The efficacy of golimumab against non-infectious uveitis: a PRISMA-compliant systematic review and meta-analysis. Ocul. Immunol. Inflamm. 31, 1013–1023 (2023).
Tungsattayathitthan, U. et al. Efficacy of golimumab in patients with refractory non-infectious panuveitis. Sci. Rep. 14, 2179 (2024).
Rudwaleit, M. et al. Observed incidence of uveitis following certolizumab pegol treatment in patients with axial spondyloarthritis. Arthritis Care Res. 68, 838–844 (2016).
van der Horst-Bruinsma, I. E. et al. Reduction of anterior uveitis flares in patients with axial spondyloarthritis on certolizumab pegol treatment: final 2-year results from the multicenter phase IV C-VIEW study. Ther. Adv. Musculoskelet. Dis. 13, 1759720x211003803 (2021).
Foster, C. S. et al. Efficacy of etanercept in preventing relapse of uveitis controlled by methotrexate. Arch. Ophthalmol. 121, 437–440 (2003).
Brito-Zerón, P., Perez-Alvarez, R. & Ramos-Casals, M. Etanercept and uveitis: friends or foes? Curr. Med. Res. Opin. 31, 251–252 (2015).
Levy-Clarke, G. et al. Expert panel recommendations for the use of anti-tumor necrosis factor biologic agents in patients with ocular inflammatory disorders. Ophthalmology 121, 785–796.e3 (2014).
McHarg, M. et al. Anti-drug antibodies to monoclonal TNF inhibitors in non-infectious uveitis. Investig. Ophthalmol. Vis. Sci. 63, 3194 – A0420–3194 – A0420 (2022).
Leinonen, S. T., Aalto, K., Kotaniemi, K. M. & Kivelä, T. T. Anti-adalimumab antibodies in juvenile idiopathic arthritis-related uveitis. Clin. Exp. Rheumatol. 35, 1043–1046 (2017).
Baert, F. et al. Influence of immunogenicity on the long-term efficacy of infliximab in Crohn’s disease. N. Engl. J. Med. 348, 601–608 (2003).
Aeschlimann, F. A. et al. Prevalence of anti-infliximab antibodies and their associated co-factors in children with refractory arthritis and/or uveitis: a retrospective longitudinal cohort study. J. Rheumatol. 44, 334–341 (2017).
Valdes, L. et al. Anti-infliximab antibodies and clinical response in noninfectious uveitis and scleritis patients treated with infliximab: a retrospective review. Am. J. Ophthalmol. Case Rep. 27, 101634 (2022).
Kreps, E. O. et al. Infliximab in chronic non-infectious paediatric uveitis refractory to previous biologic therapy. Eye 38, 871–876 (2024).
Dick, A. D. et al. Secukinumab in the treatment of noninfectious uveitis: results of three randomized, controlled clinical trials. Ophthalmology 120, 777–787 (2013).
Letko, E. et al. Efficacy and safety of intravenous secukinumab in noninfectious uveitis requiring steroid-sparing immunosuppressive therapy. Ophthalmology 122, 939–948 (2015).
Beltrán Catalán, E. et al. SER recommendations for the treatment of uveitis. Reumatol. Clín. 19, 465–477 (2023).
Brown, M. A. et al. Low uveitis rates in patients with axial spondyloarthritis treated with bimekizumab: pooled results from phase 2b/3 trials. Ann. Rheum. Dis. https://doi.org/10.1136/ard-2024-225933 (2024).
Hassan, M. et al. Utilisation of composite endpoint outcome to assess efficacy of tocilizumab for non-infectious uveitis in the STOP-Uveitis Study. Br. J. Ophthalmol. 107, 1197–1201 (2023).
Sepah, Y. J. et al. Primary (month-6) outcomes of the STOP-uveitis study: evaluating the safety, tolerability, and efficacy of tocilizumab in patients with noninfectious uveitis. Am. J. Ophthalmol. 183, 71–80 (2017).
Ramanan, A. V. et al. Tocilizumab in patients with anti-TNF refractory juvenile idiopathic arthritis-associated uveitis (APTITUDE): a multicentre, single-arm, phase 2 trial. Lancet Rheumatol. 2, e135–e141 (2020).
Heissigerová, J. et al. Efficacy and safety of sarilumab for the treatment of posterior segment noninfectious uveitis (SARIL-NIU): the phase 2 SATURN study. Ophthalmology 126, 428–437 (2019).
Schauwvlieghe, P. P., Van Calster, J., Herbort, C. P. Jr., Kestelyn, P. A. & de Vlam, K. Efficacy and safety of abatacept to treat active birdshot uveitis: a prospective open label interventional proof-of-concept trial. Br. J. Ophthalmol. 108, 244–252 (2024).
Ng, C. C., Sy, A. & Cunningham, E. T. Jr. Rituximab for non-infectious uveitis and scleritis. J. Ophthalmic Inflamm. Infect. 11, 23 (2021).
Wen, J. et al. Role of Janus kinase (JAK) inhibitor in autoimmune ocular inflammation: a systematic review. J. Immunol. Res. 2021, 2324400 (2021).
Srivastava, S. K. et al. Filgotinib in active noninfectious uveitis: the HUMBOLDT randomized clinical trial. JAMA Ophthalmol. 142, 789–797 (2024).
Ramanan, A. V. et al. Adalimumab plus methotrexate for uveitis in juvenile idiopathic arthritis. N. Engl. J. Med. 376, 1637–1646 (2017).
Quartier, P. et al. ADJUVITE: a double-blind, randomised, placebo-controlled trial of adalimumab in early onset, chronic, juvenile idiopathic arthritis-associated anterior uveitis. Ann. Rheum. Dis. 77, 1003–1011 (2018).
Acharya, N. R. et al. Discontinuing adalimumab in patients with controlled juvenile idiopathic arthritis-associated uveitis (ADJUST-Adalimumab in Juvenile Idiopathic Arthritis-associated Uveitis Stopping Trial): study protocol for a randomised controlled trial. Trials 21, 887 (2020).
Horton, S. et al. Adalimumab in juvenile idiopathic arthritis-associated uveitis: 5-year follow-up of the Bristol participants of the SYCAMORE Trial. Am. J. Ophthalmol. 207, 170–174 (2019).
Kahn, P., Weiss, M., Imundo, L. F. & Levy, D. M. Favorable response to high-dose infliximab for refractory childhood uveitis. Ophthalmology 113, 860–864.e862 (2006).
Lerman, M. A. et al. Response of pediatric uveitis to tumor necrosis factor-α inhibitors. J. Rheumatol. 40, 1394–1403 (2013).
Tappeiner, C. et al. Evidence for tocilizumab as a treatment option in refractory uveitis associated with juvenile idiopathic arthritis. J. Rheumatol. 43, 2183–2188 (2016).
Ramanan, A. V. et al. A phase II trial protocol of Tocilizumab in anti-TNF refractory patients with JIA-associated uveitis (the APTITUDE trial). BMC Rheumatol. 2, 4 (2018).
International Clinical Trials Registry Platform. A study to see whether adalimumab or secukinumab is better for treating children and young people with juvenile idiopathic arthritis (JIA) associated uveitis or chronic anterior uveitis. WHO https://trialsearch.who.int/Trial2.aspx?TrialID=ISRCTN12427150 (2023).
Ramanan, A. V. et al. Clinical effectiveness and safety of baricitinib for the treatment of juvenile idiopathic arthritis-associated uveitis or chronic anterior antinuclear antibody-positive uveitis: study protocol for an open-label, adalimumab active-controlled phase 3 clinical trial (JUVE-BRIGHT). Trials 22, 689 (2021).
ET, E. C. & Zierhut, M. Vision loss in uveitis. Ocul. Immunol. Inflamm. 29, 1037–1039 (2021).
Tomkins-Netzer, O. et al. Long-term clinical outcome and causes of vision loss in patients with uveitis. Ophthalmology 121, 2387–2392 (2014).
Ostrovsky, M. et al. Ocular Behçet disease — clinical manifestations, treatments and outcomes according to age at disease onset. Biomedicines 11, 624 (2023).
Al-Ani, H. H., Sims, J. L. & Niederer, R. L. Long term complications and vision loss in HLA-B27 uveitis. Eye 37, 1673–1677 (2023).
Niederer, R. L., Sharief, L., Tomkins-Netzer, O. & Lightman, S. L. Uveitis in sarcoidosis - clinical features and comparison with other non-infectious uveitis. Ocul. Immunol. Inflamm. 31, 367–373 (2023).
Suhler, E. B. et al. Long-term safety and efficacy of adalimumab in patients with noninfectious intermediate uveitis, posterior uveitis, or panuveitis. Ophthalmology 128, 899–909 (2021).
Jaffe, G. J., Pavesio, C. E. & Study, I. Effect of a fluocinolone acetonide insert on recurrence rates in noninfectious intermediate, posterior, or panuveitis: three-year results. Ophthalmology 127, 1395–1404 (2020).
Royal College of Ophthalmologists & British Society for Paediatric and Adolescent Rheumatology (BSPAR). Guidelines for screening for uveitis in juvenile idiopathic arthritis (JIA). https://www.rcophth.ac.uk/resources-listing/guidelines-for-screening-for-uveitis-in-juvenile-idiopathic-arthritis-jia/ (2006).
Wennink, R. A. W. et al. Improved clinical outcomes in patients with juvenile idiopathic arthritis associated uveitis in the last decade. Acta Ophthalmol. 100, 781–787 (2022).
Cann, M. et al. Outcomes of non-infectious Paediatric uveitis in the era of biologic therapy. Pediatr. Rheumatol. Online J. 16, 51 (2018).
Paroli, M. P. et al. Persistence of juvenile idiopathic arthritis-associated uveitis in adulthood: a retrospective study. J. Clin. Med. 11, https://doi.org/10.3390/jcm11092471 (2022).
Tordoff, M. et al. O01 Genetic risk factors associated with increased risk of uveitis in patients with juvenile idiopathic arthritis. Rheumatology 60, https://doi.org/10.1093/rheumatology/keab246 (2021).
Invernizzi, A. et al. Objective quantification of anterior chamber inflammation: measuring cells and flare by anterior segment optical coherence tomography. Ophthalmology 124, 1670–1677 (2017).
Tsui, E. et al. Quantification of anterior chamber cells in children with uveitis using anterior segment optical coherence tomography. Am. J. Ophthalmol. 241, 254–261 (2022).
Sorkhabi, M. A., Potapenko, I. O., Ilginis, T., Alberti, M. & Cabrerizo, J. Assessment of anterior uveitis through anterior-segment optical coherence tomography and artificial intelligence-based image analyses. Transl. Vis. Sci. Technol. 11, 7 (2022).
Solebo, A. L., Bellchambers, A., Kellett, S., Rahi, J. S. & Dick, A. D. Establishing the normative data set necessary for imaging-based childhood uveitis surveillance: a cross-sectional study. Invest. Ophthalmol. Vis. Sci. 65, 9 (2024).
Garcia-Onrubia, L. et al. Tear and plasma levels of cytokines in patients with uveitis: search for active disease biomarkers. J. Clin. Med. 11, 7034 (2022).
Angeles-Han, S. T. et al. S100 proteins, cytokines, and chemokines as tear biomarkers in children with juvenile idiopathic arthritis-associated uveitis. Ocul. Immunol. Inflamm. 29, 1616–1620 (2021).
Pato, E. et al. Development of an activity disease score in patients with uveitis (UVEDAI). Rheumatol. Int. 37, 647–656 (2017).
Pato-Cour, E. et al. Validation of UVEDAI: an index for evaluating the level of inflammatory activity in uveitis. Ophthalmol. Ther. 12, 1045–1055 (2023).
Yuan, P. D. et al. Adalimumab dose reduction and withdrawal in stable non-infectious pediatric uveitis: an open-label, prospective, pilot study. Ocul. Immunol. Inflamm. https://doi.org/10.1080/09273948.2024.2343084 (2024).
Iapoce, C. NEPTUNE: brepocitinib displays strong efficacy in non-infectious uveitis. HCPLive https://www.hcplive.com/view/neptune-brepocitinib-displays-strong-efficacy-non-infectious-uveitis (2 April 2024).
Klint, S. et al. Izokibep: preclinical development and first-in-human study of a novel IL-17A neutralizing Affibody molecule in patients with plaque psoriasis. MAbs 15, 2209920 (2023).
Bang, C. H. et al. Ustekinumab demonstrates lower uveitis risk in moderate to severe psoriasis patients compared with tumor necrosis factor-α inhibitors. Acta Derm. Venereol. 104, adv34206 (2024).
Roche. Vamikibart in participants with uveitic macular edema. ForPatients by Roche https://forpatients.roche.com/en/trials/eye-disorder/uveitic-macular-edema/ro7200220-in-participants-with-uveitic-macular-edema-91001.html#formedicalprofessionals (2024).
Gelfman, S. et al. A large meta-analysis identifies genes associated with anterior uveitis. Nat. Commun. 14, 7300 (2023).
Burgess, S. et al. Using genetic association data to guide drug discovery and development: review of methods and applications. Am. J. Hum. Genet. 110, 195–214 (2023).
Wu, K. Y., Tan, K., Akbar, D., Choulakian, M. Y. & Tran, S. D. A new era in ocular therapeutics: advanced drug delivery systems for uveitis and neuro-ophthalmologic conditions. Pharmaceutics 15, https://doi.org/10.3390/pharmaceutics15071952 (2023).
Rebibo, L. et al. Topical tacrolimus nanocapsules eye drops for therapeutic effect enhancement in both anterior and posterior ocular inflammation models. J. Control. Rel. 333, 283–297 (2021).
Author information
Authors and Affiliations
Contributions
The authors contributed equally to all aspects of the article.
Corresponding author
Ethics declarations
Competing interests
S.L.N.C. declares that they are a full-time employee of AstraZeneca.
Peer review
Peer review information
Nature Reviews Rheumatology thanks James Rosenbaum, Melissa Lerman and Sheila Angeles-Han for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Related links
Glossary
- Anterior uveitis
-
Inflammation of the front part of the eye, which includes the iris and surrounding tissue, and causes redness, pain, photophobia and blurred vision.
- Band keratopathy
-
A condition in which calcium deposits form on the cornea, the clear front part of the eye, causing a band-like appearance and potentially affecting vision.
- Flare
-
The presence of proteins in the aqueous humour, the clear fluid in the front part of the eye, indicates inflammation, which can cause the fluid to appear cloudy.
- Glaucoma
-
A group of eye conditions that damage the optic nerve, often owing to high pressure inside the eye; glaucoma can lead to vision loss or blindness if untreated.
- Intermediate uveitis
-
Inflammation that affects the middle part of the eye, including the vitreous humour (the gel-like substance filling the eye), symptoms of intermediate uveitis can include floaters and blurred vision.
- logMAR
-
A logarithmic notation used to express visual acuity (clarity of vision) in which lower scores correspond to better vision; logMAR is a more precise way of measuring visual acuity than the traditional Snellen chart.
- Macular oedema
-
Swelling or fluid build-up in the macula, the central part of the retina, responsible for detailed vision, that can cause distorted or blurred vision.
- Panuveitis
-
Inflammation affecting all parts of the uvea (the middle layer of the eye), including the iris, ciliary body, and choroid, that can cause widespread vision problems.
- Posterior synechiae
-
Adhesions between the iris and the lens of the eye, often as a result of inflammation, that can lead to irregular pupil shape and other vision issues.
- Posterior uveitis
-
Inflammation of the back part of the eye, including the retina and choroid; symptoms of posterior uveitis can include blurred vision, floaters and sometimes pain.
- Standardization of Uveitis Nomenclature
-
(SUN). Standardized guidelines developed by SUN Working Group to classify and describe uveitis for consistent diagnosis and treatment.
- Visual acuity
-
A measure of the clarity or sharpness of vision, often assessed using an eye chart (see logMAR), that indicates how well a person can see details at a specific distance.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Clarke, S.L.N., Maghsoudlou, P., Guly, C.M. et al. The management of adult and paediatric uveitis for rheumatologists. Nat Rev Rheumatol 20, 795–808 (2024). https://doi.org/10.1038/s41584-024-01181-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41584-024-01181-x