In the early 1980s, Channing Der was just beginning his career as a scientist at Harvard Medical School when he happened upon a discovery that would change the course of cancer research. At the time, the holy grail of cancer biology was discovering so-called oncogenes – genetic switches that can turn a normal cell into a cancer cell – in the genomes of tumours. But while teams of scientists had thrown everything at it for the best part of a decade, their efforts had proved fruitless. One by one, they were beginning to accept that it might be a dead end.
Der found himself assigned to test 20 different genes that had been identified as possible oncogene candidates. His question was simple: did any of them actually exist in tumours in a form that was different from normal cells?
“People thought it wasn’t going to work,” he remembers. “I began, and certainly for five months, the chances of success seemed to be pretty slim. I was ready to just wrap this up, and move on to something else that might be more productive, when I made the discovery which changed the course of my professional career.”
The first 18 of the genes Der tested turned out to be normal. But the final two, members of a gene family called RAS, were found to be uniquely mutated in cancer cells. “Being fairly new to the field at that point, I didn’t fully understand the ramifications of what this meant,” he laughs. “I was working in the lab of a professor named Geoffrey Cooper, and when I showed him the results, he paused for what seemed like minutes. So I asked if he was OK, and he replied: ‘This could be one of the most significant discoveries in cancer biology in decades.’”
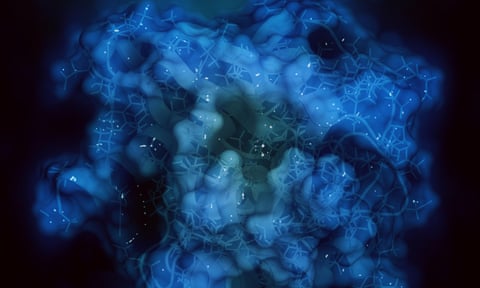
We now know that about 20% of all cancers harbour a mutation in one of three RAS genes; KRAS, HRAS and NRAS. Each of these genes directs the production of a protein that naturally flexes and relaxes, on and off, thousands of times a second. In the “on” position, it allows cells to grow, and then in the “off” setting, it stops the growth. However, when the RAS genes are mutated, the protein remains stuck in its on state, and the cell is forced to proliferate out of control, becoming a tumour. Of the three genes, KRAS is the most notorious, as its mutant forms are commonly found in some of the deadliest cancers. KRAS mutations occur in up to 96% of pancreatic cancers, and 54% of colorectal cancers.
Over the past 40 years, the pharmaceutical industry has repeatedly tried to find a way to switch RAS proteins off in cancer cells. It has been a long journey, checkered with abandoned hopes, and hundreds of millions lost in failed trials. But over the past eight years, a breakthrough has breathed new light into the field. At least eight companies now have drugs in clinical development that appear to successfully target a KRAS mutant. If all goes to plan in 2021, they could soon be approved by regulators, paving the way for a whole new class of cancer medicines.
Back in the 1980s, it was not long before the early optimism surrounding RAS began to fade. “Virtually every major pharma company put their hat in the ring and said, ‘We’re going after this,’” says Der. “With time more ideas came up, more ideas were tried, and more ideas failed. It was the best of times, and then it became the worst of times for RAS drug discovery.”
Scientists wanted to find drugs that could attach to RAS proteins and hold them permanently in the off state, but they swiftly realised this was far from easy. The proteins were often likened to tennis balls, and it was seemingly impossible to find anything that could bind to them. “We like to call KRAS the Death Star,” says David Reese, executive vice-president for research and development at Amgen, who has been involved in RAS drug discovery since the 1990s. “It’s spherical and impenetrable. Proteins usually have nooks and crannies which you use to latch on to. This was a huge challenge for chemists because drugs would essentially bounce off.”
However in the early 1990s, scientists thought they had cracked the problem. All RAS proteins have a fatty tail, created by an enzyme called farnesyl transferase, with which they latch on to the cancer cell membrane. Blocking this enzyme seemed like a surefire way of stopping RAS proteins from working.
Initially it seemed like a perfect strategy, especially when the drugs successfully halted cancer growth in mice. Der recalls that six major pharmaceutical companies were sufficiently convinced to then gamble vast sums on clinical trials. But one by one, the drugs failed. It transpired that human cancer cells have a contingency plan. RAS proteins, it turns out, contain an enzyme that can create a new fatty tail if farnesyl transferase isn’t functioning. It rendered the experimental drugs useless.
Wounded by the failure, many scientists walked away from the field, and RAS proteins soon came to be seen as undruggable. “People certainly became disillusioned,” says Der. “At that point I saw many pharma companies simply say: ‘This is too tough, let’s go look for something else.’”
But 20 years later, the field would be suddenly revitalised, thanks to the determination of one academic chemist.
In 1999, Kevan Shokat arrived in San Francisco to begin collaborating with a cancer researcher called Frank McCormick. Despite Shokat’s initial misgivings, McCormick urged him to look for a new method of drugging the KRAS protein that was behind so many lethal cancers.
“Even though I told him I couldn’t think of a way to do that, he kept encouraging me, and inviting RAS experts from all over the world to give talks,” says Shokat. “As drug discovery evolved, things fell in place for us to take a stab at it.”
By the late 2000s, Shokat had become interested in one particular KRAS mutant called G12C. This is found in 13% of patients with non-small cell cancer, the most common form of lung cancer, as well as 3% of colorectal cancer patients. Over the next five years, Shokat and colleagues would screen around 500 different molecules to see if any could latch on to G12C.
In 2013, their persistence paid off. To Shokat’s amazement, one particular drug had achieved the seemingly impossible. It had created a tiny groove in the protein’s surface, and used it to hold G12C steady. “The drug was sitting in a beautiful pocket that no one had ever seen on the protein,” he remembers.
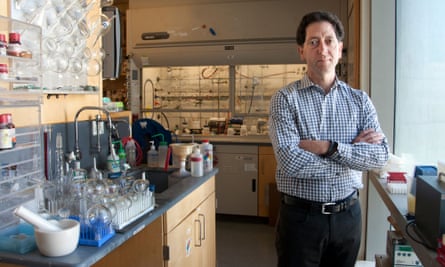
It was the biggest breakthrough in RAS biology in years. For the first time in almost two decades, the pharmaceutical industry began to take note again. “A lot of us started thinking, maybe this groove in G12C is like a little hook that a mountain climber would use, somewhere to put your fingertips, and grasp on to,” says Reese.
Inspired by Shokat’s breakthrough, more than eight companies around the world, from Amgen to Johnson & Johnson, began to design and test their own inhibitors against G12C. In 2019, the watershed moment came when Amgen scientists presented the first human trial results of their inhibitor sotorasib in advanced lung cancer patients.
“There were 40,000 oncologists from around the world gathering in Chicago to review the latest data,” recalls Reese. “Usually the new drug development session is a sleepy backwater of this conference, but this time, the room was overflowing with people, and you could feel the electricity when the data was presented.”
The excitement was justified. In those early readouts, sotorasib was found to be capable of both shrinking solid tumours, and delaying disease progression after six weeks of treatment. Last month, Amgen released the data from a much larger patient cohort, after following them for a year. It was found that 37% had either complete or partial tumour shrinkage, while 81% saw their condition stabilise.
Der points out that the tumour shrinkage is a key result. “If the tumour mass is too large, you can’t operate,” he said. “If you can shrink the tumour, that patient might now be a candidate for surgery, and at the end of the day, our best treatment for cancer is still surgical resection of the tumour. That is what cures people.”
Amgen is not the only company to report promising clinical trial data. Last October, Mirati Therapeutics released data from early stage trials of their G12C inhibitor adagrasib, which helped shrink tumours in 45% of advanced lung cancer patients. However, both Amgen and Mirati have had less success when using their inhibitor against colorectal cancer patients with the G12C mutation.
In December 2020, Amgen asked the Food and Drug Administration and the European Medicines Agency to review sotorasib, leading to anticipation that it could be approved later this year as a new therapy for certain lung cancer patients. In the eyes of many oncologists, this would be a welcome weapon against a disease that remains notoriously difficult to treat.
“Lung cancer is still extremely challenging clinically, and affects a very large number of patients, being the commonest cause of cancer deaths worldwide,” says Julian Downward, a cancer researcher at the Francis Crick Institute. “Improvements in therapies in the past decade have come from two areas. One is the development of receptor tyrosine kinase inhibitors, which are effective in some 10% or so of lung cancer patients. The other has been the development of immunotherapies. These can work very well in some patients but unfortunately it is only a minority. So there is still a huge unmet need in the treatment of lung cancer and it is to be hoped that at least part of that might be met by these new KRAS drugs.”
However, neither sotorasib nor any of the other G12C inhibitors in development are miracle cures. In many patients, the best prognosis will be that they prolong life by months, or increase quality of life, even though patients remain terminally ill. Cancer is a versatile foe, quick to adapt to anything thrown at it. Even the most optimistic researchers agree that the benefits offered by G12C inhibitors will only be fleeting, and tumours will quickly develop workarounds.
“We’ve learned from past experiences that virtually every cancer treatment will be limited by resistance,” says Der. “The cancer cell is rather an amazing beast in that it is built to survive, and one of the characteristics of cancer cells is that they seem to overcome everything we throw at them. So these G12C inhibitors are not an exception. The cancer cells will find some way of overcoming the drug and growing again.”
Still, the development of G12C inhibitors has reignited commercial and academic interest in a field that was long considered hopeless. Amgen and others are investigating whether pairing their inhibitors with immunotherapies can make them more effective, while Moderna is exploring whether a cancer vaccine targeting multiple KRAS mutations simultaneously could address the problem of tumour resistance. Interest is also turning towards designing inhibitors against another KRAS mutant called G12D, which is the most prevalent KRAS mutant in cancer.
“People are now saying, if we could do this trick with G12C mutations, why can’t we do it with other RAS mutations,” says Der. “Inhibiting G12D would be even bigger. Having developed these inhibitors is a groundbreaking moment in cancer biology.”