Abstract
Purpose
Intubation-associated trauma with the GlideScope is rare, but when it occurs, it is likely due to advancing the endotracheal tube (ETT) blindly between the direct view of the oropharynx and the video view of the glottis. It is also occasionally difficult to advance the ETT to the glottic aperture despite a good view of the glottis on the monitor. One technique to potentially address both issues is to introduce the ETT en bloc with the GlideScope, thus visualizing the ETT tip throughout its entire path. We hypothesized that this en bloc technique could be faster and potentially easier than the standard technique.
Methods
Fifty patients with normal-appearing airways who required orotracheal intubation for elective surgery were randomly allocated to intubation with either the en bloc or the standard (GlideScope-first-then-ETT) technique. A three-dimensional printed clip was utilized to secure the ETT to the GlideScope during en bloc insertion. The primary outcome was time to intubation, defined from mask removal to first end-tidal carbon dioxide detection, recorded by a blinded observer. Secondary outcomes were subjective ease of intubation (100-mm visual analogue scale [VAS], 0 = easy; 100 = difficult), number of intubation attempts/failures, and incidence of oropharyngeal trauma (bleeding).
Results
The median [interquartile range (IQR)] intubation time was 36 [31–42] sec with the en bloc technique vs 41 [37–50] sec with the standard technique (difference in medians, 5 sec; 95% confidence interval [CI], 2 to 11; P = 0.008). The median [IQR] ease of intubation VAS was 11 [9–21] mm with the en bloc technique, and 15 [11–24] mm with the standard technique (difference in medians, 4 mm; 95% CI, −2 to 8; P = 0.19). Laryngoscopic grade and number of intubation attempts were similar between the groups; there was no oropharyngeal trauma noted.
Conclusion
In this study of video laryngoscopy, intubation was slightly faster with the en bloc technique than with the standard GlideScope intubation technique, although the clinical importance of this difference is unknown.
Trial registration
www.clinicaltrials.gov (NCT02787629); registered 1 June 2016.
Résumé
Objectif
Les traumatismes associés à l’intubation avec un GlideScope sont rares; quand ils surviennent, ils sont souvent provoqués par l’insertion du tube endotrachéal (TET) en aveugle entre la visualisation directe de l’oropharynx et la visualisation par vidéo de la glotte. Il arrive parfois qu’il soit difficile d’insérer le TET dans l’ouverture glottique malgré une bonne visualisation de la glotte sur le moniteur. Une technique permettant potentiellement de résoudre ces deux problèmes est l’introduction ‘en bloc’ du TET et du GlideScope, de manière à obtenir une vue de l’extrémité du TET tout au long de son parcours. Nous avons émis l’hypothèse que cette technique en bloc pourrait être à la fois plus rapide et potentiellement plus facile à réaliser que la technique standard.
Méthode
Cinquante patients présentant des voies aériennes d’apparence normale et nécessitant une intubation orotrachéale pour une chirurgie non urgente ont été randomisés à être intubés soit par une technique en bloc, soit en utilisant la technique standard (GlideScope puis TET). Une pince imprimée en 3D a été utilisée pour attacher le TET au GlideScope pendant l’insertion en bloc. Le critère d’évaluation principal était le temps nécessaire à l’intubation, défini à partir du moment de retrait du masque jusqu’à la première détection de dioxyde de carbone télé-expiratoire, tel que mesuré par un observateur en aveugle. Les critères secondaires comprenaient la facilité subjective d’intubation (sur une échelle visuelle analogique [EVA] de 100 mm, où 0 = facile et 100 = difficile), le nombre de tentatives et d’échecs d’intubation, et l’incidence de lésions oropharyngées (saignement).
Résultats
Le temps d’intubation médian [écart interquartile (ÉIQ)] était de 36 [31–42] sec avec la technique en bloc vs 41 [37–50] sec avec la technique standard (différence de moyennes, 5 sec; intervalle de confiance [IC] 95 %, 2 à 11; P = 0,008). La facilité d’intubation médiane [ÉIQ] sur l’EVA était de 11 [9-21] mm avec la technique en bloc, et 15 [11-24] mm avec la technique standard (différence de moyennes, 4 mm; IC 95 %, -2 à 8; P = 0,19). La classification de la laryngoscopie et le nombre de tentatives d’intubation étaient similaires dans les deux groupes; aucun traumatisme oropharyngé n’a été enregistré.
Conclusion
Dans cette étude vidéolaryngoscopique, l’intubation était légèrement plus rapide lors de l’utilisation de la technique en bloc que lors d’une technique d’intubation standard avec le GlideScope, bien que l’importance clinique de cette différence soit inconnue.
Enregistrement de l’étude
www.clinicaltrials.gov (NCT02787629); enregistrée le 1er juin 2016.
Similar content being viewed by others
The GlideScope® Titanium™ video laryngoscope (Verathon Medical Inc., Bothell, WA, USA) uses a high-resolution camera and LED illumination embedded into a metal laryngoscope blade. The GlideScope consistently1,2,3,4,5 provides a good laryngoscopic view6 and is routinely used for tracheal intubation.1,2,3,4,5 It has been shown to improve glottic view for orotracheal intubation compared with Macintosh direct laryngoscopy1,5 and has become a staple for advanced and emergent airway management.7,8
Nevertheless, two observations have emerged with GlideScope (and other video laryngoscope) use. The first is rare airway trauma to the palate and/or tonsillar pillars.9,10,11,12,13,14,15 With standard use, the GlideScope is inserted into the pharynx and a glottic view obtained, after which the endotracheal tube (ETT) is advanced. While the ETT can be visualized directly in the oral cavity, and subsequently at the glottic aperture via the GlideScope screen, a portion of the ETT advancement is done blindly, and this may contribute to airway trauma.9,12,13,15 The second observation is that it is occasionally difficult to advance the ETT to a position at the glottic aperture visible on the monitor,16,17,18 even with a good view6 of the glottis.
To address both of these concerns, a technique can be used where the ETT is inserted simultaneously (i.e., en bloc) with the GlideScope blade. The ETT and blade can be observed directly in the oral cavity and the ETT tip can then be continually visualized on the GlideScope monitor as it is advanced to the glottis. It is self-evident that advancing the ETT under visual guidance will be safer than blind advancement, but it is unknown if this technique would take longer. With respect to potential difficult ETT advancement despite a good glottic view, the challenge is often in maneuvering the ETT tip into the view seen on the monitor. With the ETT advanced en bloc, the ETT tip remains on the monitor throughout the process; when the glottis is visualized, the ETT is adjacent and easier to advance into the trachea, having eliminated any blind advancement. In addition, it was postulated that with changing from a technique that traditionally involves the ETT moving from outside the mouth to an endotracheal position to one where the ETT only has to pass through the vocal cords, that the overall intubation sequence could potentially be faster.
This en bloc technique is different from channelled7 video laryngoscopes (such as the AirTrac®), which include an ETT tube channel integrated into the laryngoscope blade. These devices require movement of the video laryngoscope at the expense of glottic view, to maneuver the ETT during advancement. With the en bloc technique, the ETT is only secured in the monitor view during the advancement of the video laryngoscope; the ETT is then released and maneuvered independently while being advanced through the cords, while the video laryngoscope (and monitor view) is kept steady.
There has been no study to date comparing en bloc ETT insertion to the standard GlideScope video laryngoscope-first technique. Prior to conducting a larger multi-operator study, this single-blinded single-operator preliminary study hypothesized that the en bloc technique could be faster than the standard technique. The secondary hypothesis was that the technique would also be easier.
Methods
This trial took place at two teaching hospitals in London, Ontario, Canada, from 26 October 2016 to 29 June 2018. It was registered at clinicaltrials.gov on 1 June 2016 (NCT02787629) and approved by London Health Sciences Centre and the University of Western Ontario Health Sciences Research Ethics Board (REB#107322) on 8 August 2016 prior to first patient enrollment.
Written informed consent was obtained from all patients. English-speaking adult patients, scheduled for elective surgery requiring orotracheal intubation, were invited to participate. Exclusion criteria included known or anticipated difficult airway (as judged by either the attending or pre-admission clinic anesthesiologist), cervical spine abnormality, and patients requiring rapid sequence induction. To ensure uniformity in intubation technique, all intubations were performed by one operator with experience of > 1,000 video laryngoscopic intubations.
Patient demographics and airway assessment were recorded preoperatively. At the discretion of the operator, a size 3 or 4 GlideScope Titanium blade was chosen prior to randomization. A Mallinckrodt Hi–Lo® ETT (Mallinckrodt Inc., St. Louis, MO, USA) was used in all cases. To minimize potential airway trauma, a Satin-Slip™ 14F stylet (Mallinckrodt Inc.) was used instead of the rigid GlideScope-specific stylet.19,20 The ETT size was chosen by the attending anesthesiologist before randomization. The angulation of the ETT stylet was a 90° bend at 8 cm,21,22 with the ETT cut to approximately 25 cm in length. The styleted ETT was prepared prior to the patient being allocated to a study group.
Each patient was allocated to the en bloc ETT or standard GlideScope video laryngoscope-first group by a computer-generated random code (www.random.org) in a sealed opaque envelope. It was unsealed and viewed only by an assistant prior to patient entrance into the operating room, to maintain the operator blinding until just prior to intubation. Study subjects were block randomized to 25 patients per group.
If the patient was in the en bloc group, the assistant placed the ETT and GlideScope en bloc on a Mayo stand beside the surgical table, covered by an obscuring towel. If the patient was in the standard group, the assistant placed the ETT and GlideScope loose, similarly covered. The GlideScope monitor was rotated to avoid revealing group assignment on the screen, as the ETT would appear on the screen in the en bloc group. Although towel removal and monitor repositioning added slightly more time to the subsequent intubation during the study, it was considered worthwhile to preserve blinding of the timer (and the operator during patient positioning and induction). Repositioning was identical for both groups, avoiding between-group bias. As the patient entered the room, the assistant who prepared the equipment departed and had no additional involvement in the patient’s care.
To improve external validity, all patient care aspects other than the paralytic (rocuronium ≥ 0.6 mg·kg−1) were at the discretion of the attending anesthesiologist. Patients were supine with a regular pillow under their head for intubation. After induction, patients were mask-ventilated for a minimum timed interval of 90 sec to facilitate muscle relaxation. The operator then removed the covering towel to reveal the group assignment, rotated the GlideScope screen for viewing, and performed the intubation using the assigned technique. The operator remained blinded until prior to intubation to avoid potential bias during patient positioning, induction (including medication doses selected by the blinded attending anesthesiologist), and bag-mask ventilation.
In the standard group, the operator utilized the standard technique as described by the manufacturer, inserting the GlideScope and obtaining an acceptable view as described by Gu.23 The operator introduced the ETT blindly from the visible area of the pharynx to the glottic aperture visible on the monitor, and subsequently inserted the ETT tip into the trachea. In the en bloc group, the operator inserted the GlideScope and ETT en bloc to obtain an acceptable glottic view,23 separated the ETT, and inserted the ETT tip into the trachea. The ETT tip was visualized continuously as it was advanced from outside the oral cavity into the trachea, directly while in the mouth, and on the monitor when it passed from direct view. In both groups, once the ETT tip passed the glottic aperture, the stylet was withdrawn, the ETT advanced, and the endotracheal intubation confirmed via end-tidal carbon dioxide (CO2).
Prior to beginning the study, our usual practice was to perform en bloc intubation with the GlideScope in the left hand and the ETT taped to the GlideScope. The tube was similarly taped in this study to hold the ETT in the correct position as it was advanced en bloc. On the second study patient, difficulty was encountered removing the tape that had been applied by the assistant. Thus, a plastic clip was designed to hold the ETT and preserve blinding under the towel, while remaining easy to “unclip” and advance the ETT. The tracheal tube clip (TTC) was attached to the handle portion of the GlideScope and did not enter the patient’s oral cavity. Figure 1 shows an ETT and GlideScope blade en bloc with the TTC. Just as with the original tape, the TTC was designed to match the complex curvature of the GlideScope Titanium handle and to hold the ETT such that the ETT tip remained visible in the top right corner of the screen during the entire ETT advancement. The TTC drawing/three-dimensional (3D) print files are available online (https://doi.org/10.6084/m9.figshare.12330674). The TTC was modeled and 3D printed in polylactic acid using 100% infill and a layer height of 0.2 mm, with foam to secure the ETT. Health Canada does not require additional approval for class 1 medical devices such as this, (e.g., blood pressure cuffs, ETT holders.) This is similar to US Food and Drug Administration exemptions for level 1 medical devices. The TTC was cleaned with alcohol wipes between cases.
Endotracheal tube (ETT) and GlideScope blade en bloc with the tracheal tube clip (TTC) prior to being covered by a towel. Note the view of the ETT in the top right corner of the GlideScope monitor. The ETT tip is shown with exaggerated intrusion into the monitor picture for clarity. During intubation, the ETT tip can be moved to the left or right with small external rotations of the ETT. The STL data file for three-dimensional printing is available online (https://doi.org/10.6084/m9.figshare.12330674).
The primary outcome was the time to intubation. To preserve blinding of the timer to group assignment,24 time to intubation was defined from when the face mask was removed from the patient’s face to when end-tidal CO2 (≥ 20 mmHg) was observed after intubation. Timing was initiated as soon as the mask was removed and the blinded timer then viewed only the anesthesia monitor (i.e., not the GlideScope screen or the intubation itself). If the intubation attempt took longer than 150 sec or more than three attempts, or if the patient significantly desaturated (in the opinion of the attending anesthesiologist), it would be deemed an intubation failure and the airway would be managed as deemed appropriate by the attending anesthesiologist, including crossover to the other group if desired. Ventilation between intubation attempts would be done if deemed appropriate by the attending anesthesiologist, and would be recorded as a study secondary outcome.
Other pre-specified secondary outcomes included laryngoscopic grade,6 ease of intubation (as scored by the operator immediately after laryngoscopy on a 100-mm visual analogue scale [VAS]: 0 = easy, 100 = difficult), and number of attempts. An additional attempt at intubation was defined as each time the operator removed and reinserted either the GlideScope or the ETT from the patient’s mouth. The number of attempts and need for ventilation between attempts could not be measured in a blinded manner. The intubation duration was not revealed to the operator until after the study had been completed to avoid biasing the ease of intubation score. The oropharynx was suctioned following intubation. The presence of blood was recorded as a semi-qualitative outcome by the blinded assessor as none, trace, moderate, or severe.
This completed the protocol and the remainder of the surgery proceeded in the usual fashion. Patients were extubated according to the attending anesthesiologist’s usual practice.
Statistical analysis
The null hypothesis was that there would be no difference in the time to intubation whether the en bloc or standard technique was utilized or not. For this proof-of-concept preliminary study, a convenience sample of 50 patients was selected. All analyses were conducted according to the intention-to-treat principle, by a statistician not otherwise involved in the study.24 Stata version 15 (StataCorp LLC, College Station, TX, USA) was used for all analyses. P < 0.05 was considered statistically significant. No corrections for multiple comparisons were made.25
Summary statistics were computed for baseline demographic variables. Histograms constructed for intubation duration and for ease of intubation were first assessed visually to determine if they were approximately normally distributed. Because they were not, the null hypothesis test of no difference between medians was calculated using the Mann–Whitney U test, and the Hodges–Lehmann technique was used to calculate the 95% confidence interval (CI). The intubation duration was also analyzed using the Kaplan–Meier method (and log-rank test) to graphically display the probability of being successfully intubated at any given time. Cox regression enabled estimation of the probability of being successfully intubated at any given time in the en bloc group compared with in the standard group (i.e., the hazard ratio) after verifying the proportional hazards assumption by analyzing Schoenfeld residuals (using the estat phtest in Stata). Categorical variables were analyzed using a two-sided Fisher’s exact test.
Results
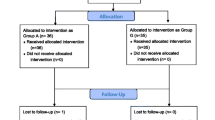
Fifty-five patients were approached to participate in the study. One patient declined and four patients consented but had their surgeries postponed, pre-empting participation. The remaining 50 patients consented, were randomized, and contributed data. Figure 2 shows a CONSORT allocation diagram illustrating patient disposition. Baseline demographics are shown in Table 1 and were similar between study groups. All patients were successfully intubated using the assigned technique.
The results are shown in Table 2 and in Fig. 3. The median [interquartile range (IQR)] intubation duration was 36 [31–42] sec with the en bloc technique vs 41 [37–50] sec with the standard technique (difference in medians, 5 sec; 95% CI, 2 to 11; P = 0.008). Figure 3 represents the laryngoscopy time data presented as a Kaplan–Meier curve, indicating the percentage of patients intubated at any point in time for each study group. The probability of being intubated at any given time in the en bloc group compared with the standard group (i.e., the hazard ratio) was 2.1 (95% CI, 1.2 to 3.8).
Laryngoscopy duration presented as a Kaplan–Meier curve showing the percentage of patients intubated vs time (log-rank P = 0.008). GVL = GlideScope. The probability of being intubated at any given time in the en bloc group vs the control group (i.e., hazard ratio) was 2.1 (95% confidence interval, 1.2 to 3.8)
The median [IQR] ease of intubation using the 100-mm VAS was 11 [9–21] mm with the en bloc technique and 15 [11–24] mm with the standard technique (difference in medians, 4 mm; 95% CI, −2 to 8; P = 0.19). There was also no statistically significant difference between the groups for number of intubation attempts, laryngoscopic grade, or incidence of oropharyngeal bleeding, as shown in Table 2. No trace, moderate, or severe bleeding was observed. No patient required ventilation between intubation attempts.
Considering that two of the patients were intubated using tape to hold the ETT instead of the TTC, a sensitivity analysis was performed after excluding these two patients. No changes to the results were observed.
Discussion
In this study of a single experienced video laryngoscope user, insertion of the ETT en bloc, advancing the ETT under vision, was feasible and was associated with a slightly faster (five seconds) intubation. While this difference was statistically significant, the clinical significance is likely only relevant for a subset of patients with longer intubation times. This suggests feasibility for this technique and that additional study to confirm these findings in a larger, multi-operator sample is warranted.
Figure 3 shows a Kaplan–Meier plot illustrating the percentage of patients who were intubated at any given time for each study group. The curves track similarly, with a fairly linear X axis (time) offset; the en bloc group is several seconds quicker. This difference likely represents the time for the ETT to be advanced from outside the oral cavity to a position near the glottic aperture, a step that is eliminated with the en bloc technique. The GlideScope insertion and subsequent ETT advancement from the aperture to endotracheal location were likely similar for both techniques.
The time-to-intubate results support the en bloc technique, (visualizing the ETT tip throughout the intubation process) as a useful technique if difficulty is encountered advancing the ETT during routine GlideScope use. The ease of intubation VAS was not statistically significantly different between the groups. Nevertheless, the results suggest that the en bloc technique is unlikely to be more difficult; this would also validate the en bloc technique as a rescue technique if it were difficult to advance the ETT with a good glottic view.
There was no observed trauma9,10,11,12,13,14,15 in either group, and while the potential benefit of visualizing the ETT for its entire path through the pharynx to the trachea is self-evident, this study was not powered to evaluate this outcome. Considering the complication rate associated with GlideScope intubation, a much larger sample size would be required to show difference in these low-probability events.
Studies comparing GlideScope intubation to direct laryngoscopy have shown that direct laryngoscopy can be faster on average than GlideScope techniques.1,3 Considering that the en bloc technique has shown the potential to allow faster GlideScope intubation, it may be prudent to reconsider this finding.
Strengths of this trial include using the maximal possible blinding, as well as a protocol to maximize external validity, considering that video laryngoscopy cannot be blinded. As this study involved patients with “normal” airways, it could potentially not be generalizable to more difficult airway cases. The study is limited by the small sample size with potential for non-reproducibility. There is also concern for limited generalizability to the intubating population in that all intubations were performed by a single very experienced operator.18 Favouring generalizability would be the fact that the operator had completed several orders of magnitude more “standard” GlideScope intubations than en bloc intubations and yet the en bloc procedure still showed benefit—most practitioners would share this greater familiarity with the standard technique. Another limitation of this trial is that it could be interpreted as having evaluated two interventions simultaneously: en bloc GlideScope and ETT advancement and the clip used to allow one-handed use. Both techniques have been used successfully by the author and it may well be that both interventions should be evaluated separately as part of larger trials. In addition, the TTC designed to hold the ETT was a first iteration designed for study blinding and could benefit from additional design optimization.
One consideration is that the study used a malleable stylet vs the rigid GlideScope stylet that is still used in a proportion of anesthesia environments. The concept for en bloc intubation would be similar for the rigid stylet, and it seems likely that the benefit of avoiding blind advancement and instead advancing the ETT under visual guidance would be even more substantive in the setting of the rigid stylet and its greater potential19,20 for trauma.9,10,11,12,13,14,15
A Hawthorne26 effect could have potentially affected the results as the operator was aware of the evaluation of potential trauma (more care/extra time), as well as the timing of the intubation (hurrying/reduced time). There could also be a (subconscious) operator bias in favour of either technique that cannot be ruled out, as double blinding is not possible for this type of airway study.
Caution is advised in extending the results to inexperienced operators, who may not be as adept at video laryngoscopic intubation. Conversely, it is also possible that this technique would be even more valuable for the inexperienced physician, as they could potentially have a higher complication rate.9,12
In summary, this study showed that the en bloc technique for inserting the ETT with the GlideScope blade was feasible and was slightly faster than routine GlideScope intubation. Avoiding blind ETT advancement, this technique also holds promise for potentially reducing the incidence of pharyngeal trauma9,10,11,12,13,14,15 associated with GlideScope intubation. We would encourage video laryngoscope manufacturers to investigate similar devices.
References
Sun DA, Warriner CB, Parsons DG, Klein R, Umedaly HS, Moult M. The GlideScope video laryngoscope: randomized clinical trial in 200 patients. Br J Anaesth 2005; 94: 381-4.
Cooper RM, Pacey JA, Bishop MJ, McCluskey SA. Early clinical experience with a new videolaryngoscope (GlideScope) in 728 patients. Can J Anesth 2005; 52: 191-8.
Xue FS, Zhang GH, Liu J, et al. The clinical assessment of Glidescope in orotracheal intubation under general anesthesia. Minerva Anestesiol 2007; 73: 451-7.
Andersen LH, Rovsing L, Olsen KS. GlideScope videolaryngoscope vs. Macintosh direct laryngoscope for intubation of morbidly obese patients: a randomized trial. Acta Anaesthesiol Scand 2011; 55: 1090-7.
Griesdale DE, Liu D, McKinney J, Choi PT. Glidescope® video-laryngoscopy versus direct laryngoscopy for endotracheal intubation: a systematic review and meta-analysis. Can J Anesth 2012; 59: 41-52.
Cormack RS, Lehane J. Difficult tracheal intubation in obstetrics. Anaesthesia 1984; 39: 1105-11.
Law JA, Broemling N, Cooper RM, et al. The difficult airway with recommendations for management-part 2: the anticipated difficult airway. Can J Anesth 2013; 60: 1119-38.
Apfelbaum JL, Hagberg CA, Caplan RA, et al. Practice guidelines for management of the difficult airway: an updated report by the American Society of Anesthesiologists Task Force on Management of the Difficult Airway. Anesthesiology 2013; 118: 251-70.
Chin KJ, Arango MF, Paez AF, Turkstra TP. Palatal injury associated with the GlideScope. Anaesth Intensive Care 2007; 35: 449-50.
Malik AM, Frogel JK. Anterior tonsillar pillar perforation during GlideScope video laryngoscopy. Anesth Analg 2007; 104: 1610-1.
Hsu WT, Hsu SC, Lee YL, Huang JS, Chen CL. Penetrating injury of the soft palate during GlideScope intubation. Anesth Analg 2007; 104: 1609-10.
Cooper RM. Complications associated with the use of the GlideScope videolaryngoscope. Can J Anesth 2007; 54: 54-7.
Amundson AW, Weingarten TN. Traumatic GlideScope(®) video laryngoscopy resulting in perforation of the soft palate. Can J Anesth 2013; 10: 210-1.
Raja J, Clyne S, Levine J, Tebbit C, Mair E. Otorhinolaryngology management of seven patients with iatrogenic penetrating injuries from GlideScope®: our experience. Clin Otolaryngol 2014; 39: 251-4.
Allencherril JP, Joseph L. Soft palate trauma induced during GlideScope intubation. J Clin Anesth 2016; 35: 278-80.
Doyle DJ. The GlideScope video laryngoscope. Anaesthesia 2005; 60: 414-5.
Niforopoulou P, Pantazopoulos I, Demestiha T, Koudouna E, Xanthos T. Video-laryngoscopes in the adult airway management: a topical review of the literature. Acta Anaesthesiol Scand 2010; 54: 1050-61.
Agrò FE, Doyle DJ, Vennari M. Use of GlideScope® in adults: an overview. Minerva Anestesiol 2015; 81: 342-51.
Turkstra TP, Harle CC, Armstrong KP, et al. The GlideScope-specific rigid stylet and standard malleable stylet are equally effective for GlideScope use. Can J Anesth 2007; 54: 891-6.
Jones PM, Loh FL, Youssef HN, Turkstra TP. A randomized comparison of the GlideRite® Rigid Stylet to a malleable stylet for orotracheal intubation by novices using the GlideScope®. Can J Anesth 2011; 58: 256-61.
Jones PM, Turkstra TP, Armstrong KP, et al. Effect of stylet angulation and endotracheal tube camber on time to intubation with the GlideScope. Can J Anesth 2007; 54: 21-7.
Dupanović M, Isaacson SA, Borovcanin Z, et al. Clinical comparison of two stylet angles for orotracheal intubation with the GlideScope video laryngoscope. J Clin Anesth 2010; 22: 352-9.
Gu Y, Robert J, Kovacs G, et al. A deliberately restricted laryngeal view with the GlideScope® video laryngoscope is associated with faster and easier tracheal intubation when compared with a full glottic view: a randomized clinical trial. Can J Anesth 2016; 63: 928-37.
Hróbjartsson A, Thomsen AS, Emanuelsson F, et al. Observer bias in randomized clinical trials with time-to-event outcomes: systematic review of trials with both blinded and non-blinded outcome assessors. Int J Epidemiol 2014; 43: 937-48.
Perneger TV. What’s wrong with Bonferroni adjustments. BMJ 1998; 316: 1236-8.
Holden JD. Hawthorne effects and research into professional practice. J Eval Clin Pract 2001; 7: 65-70.
Acknowledgement
The authors gratefully acknowledge the respiratory therapists who assisted with the study.
Author information
Authors and Affiliations
Contributions
Timothy P. Turkstra designed the study, helped design the en bloc clip, recruited patients, collected the data, reviewed the statistical analysis, and wrote the manuscript. Daniel C. Turkstra designed and drafted the GlideScope en bloc clip, reviewed the statistical analysis, and edited the manuscript. Alexander W. Pavlosky modified the en bloc clip for production, produced the en bloc clip, and edited the manuscript. Philip M. Jones performed the statistical analysis and edited the manuscript.
Ethics declarations
Disclosures
None.
Funding statement
This study was personally funded by the authors. The GlideScopes and endotracheal tubes were provided by the London Health Sciences Centre for routine clinical care.
Editorial responsibility
This submission was handled by Dr. Hilary P. Grocott, Editor-in-Chief, Canadian Journal of Anesthesia.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Turkstra, T.P., Turkstra, D.C., Pavlosky, A.W. et al. Simultaneous en bloc endotracheal tube insertion with GlideScope® Titanium™ video laryngoscope use: a randomized-controlled trial. Can J Anesth/J Can Anesth 67, 1515–1523 (2020). https://doi.org/10.1007/s12630-020-01778-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12630-020-01778-2