Once a temporary convenience, telehealth is here to stay
Multifaceted networks supporting virtual medical visits hailed as a positive legacy of pandemic
Whether you call it telehealth, telemedicine, e-health, virtual or video visits, the electronic delivery of health care services is coming into its own.
The coronavirus pandemic spurred federal, state and private insurance programs to offer more coverage of telehealth to encourage people to follow the stay-at-home rules established in mid-March 2020.
“After this last year and the benefits we’ve seen, telehealth is definitely here to stay,” said Kiran Savage-Sangwan, speaking from Sacramento. She is the executive director of the California Pan-Ethnic Health Network, a statewide health-advocacy organization.
“The way we pay for healthcare has not robustly supported telehealth in the past,” Savage-Sangwan said. “The state has taken some interim steps before making permanent policy changes. The state will be extending the flexibilities for the Medi-Cal program through the end of next year, I believe, to continue to work out some of the policy issues.”

According to the Centers for Disease Control and Prevention, the number of telehealth visits increased in the first quarter of 2020 by 50 percent, compared with the same period the year before. A single week in March 2020 showed a 154 percent increase, compared with the same period in 2019.
Behind those numbers was a massive effort among health providers to accommodate this change. Even for UC San Diego Health, a pioneer in telehealth, the quick transition required an all-hands-on-deck approach.
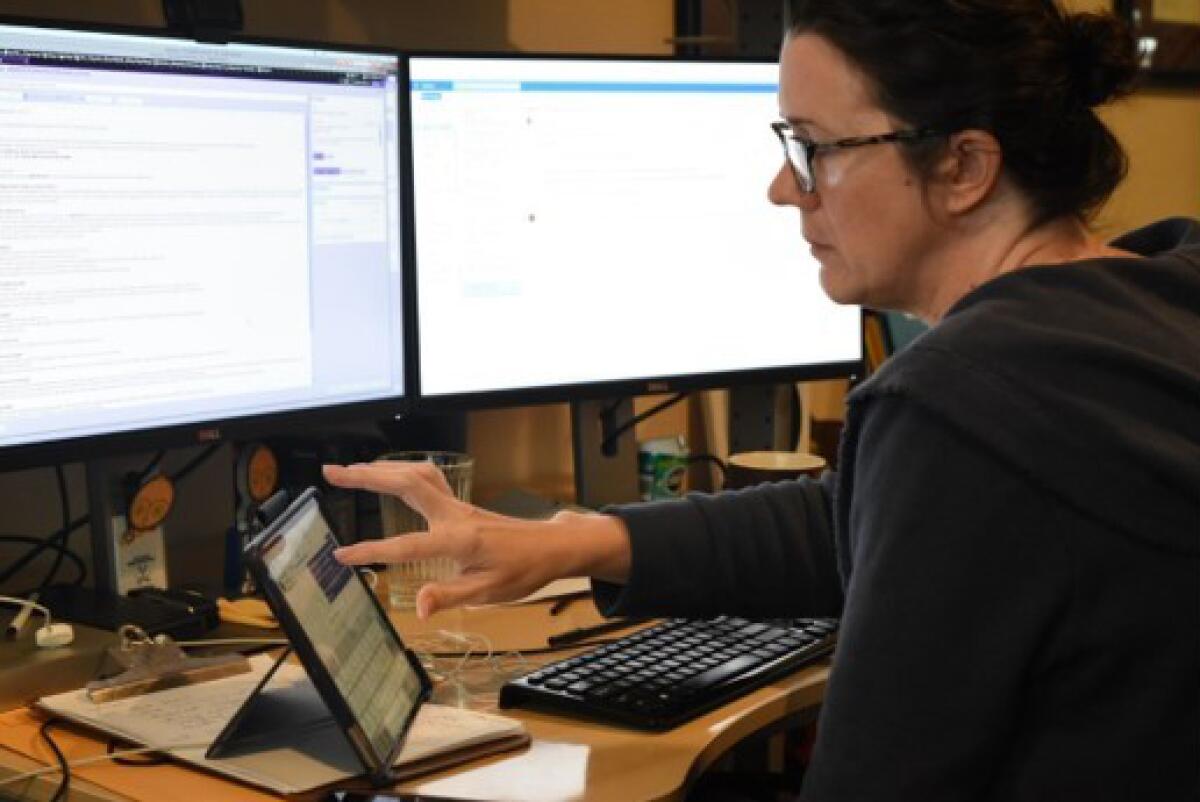
“We knew the shutdown would happen, but we didn’t know when,” recalled Marlene Millen, M.D., UC San Diego Health’s chief medical information officer for ambulatory care. “But our operational leads were already prepared for increasing video visits. Over the course of one weekend in March, we trained 1,000 doctors and staff.
“We converted appointments and sent patients instructions. That very Monday, when everyone was supposed to be locking down, we were able to convert a couple of thousand appointments into video visits. That’s because we had a really good structure in place.”
Millen spent the entire weekend at her home desk with multiple screens open, setting up online patient visits. An internal medicine physician, she has played a role in UC San Diego Health’s development of video visits for 10 years. About two or three years ago, she said, an app-based program was launched, which made it more accessible.
But it wasn’t until the insurance coverage changed that telehealth’s potential could be tested. Until the shutdown, video visits were used for patients who had extreme obstacles to making in-person appointments.
“Patients we targeted for these visits were ones with medical conditions who couldn’t come into the clinic,” Millen said. “They really embraced it. I had a patient in a wheelchair that had to be carried out of the house and another with a condition that made her use the bathroom all the time. Others had immune conditions. Then there were people who had to get on three buses to get to us.
“Some of those patients were in danger of getting kicked out of insurance because of their number of no-shows. Video visits improved those situations. But it wasn’t a general-use case at that time.”
Support for telehealth
Now that pandemic restrictions have eased, the percentage of telehealth appointments versus in-person consultations has decreased in most of California. At UC San Diego Health, Millen noted, video visits rose to 30 percent during the early 2021 surge in COVID-19 cases. Video visits now account for between 15 and 20 percent of all appointments, a figure higher than prepandemic rates.
As headlines attested, the pandemic put socioeconomic disparities in access to health care in stark relief. Some believe telehealth could provide a way to distribute health access more equitably.
But there are hurdles. Many low-income people live in Wi-Fi deserts. Some have limited minutes on their smartphones, and others are unfamiliar with the technology. For some, finding a quiet private place in a multiperson home can be a challenge.
“California has significant disparities — particularly by race, language and region — when it comes to health care access and health care outcomes,” Savage-Sangwan said. “Certainly, telehealth was helpful during the pandemic.
“When people go into a medical office, various medical professionals assist them. Someone checks you in, someone takes your weight. People support you through the process. But when you’re accessing virtual care from home, you’re going to need to get that support a different way.
“What we’ve seen to be successful is for the providers’ offices to build that into their workflow. Maybe someone calls you about your doctor’s appointment and would say: `’Hey, are you set up? Do you know how to use the platform? Let me walk you through it.’ We need to support people, so they are truly engaged in their health.”
What’s telehealth friendly?
Colonoscopies, mammograms and MRIs are obviously not possible through telehealth (at least not yet). But a lot can get done through a video visit, including assessing a medical problem and prescribing remedies for it.
Millen, of UC San Diego Health, said her telehealth patients usually followed through on her instructions. She also noted that caregivers and family members became more engaged in video visits, particularly when she asked them to help with the exam.
From monitoring diabetes and diagnosing a sinus infection to doing preliminary neurological tests and conducting speech therapy sessions, the use of telehealth has been wide ranging.
“Before the pandemic, I would have definitely said: `’Yeah, there are some specialties that won’t be able to do video visits at all,’ ” Millen observed. “I was surprised how well our doctors and staff figured out how to get patient history and information.”
Both Millen and Savage-Sangwan of the California Pan-Ethnic Health Network think that behavioral health and counseling services are extremely telehealth friendly.
Savage-Sangwan pointed out that the network’s community clinics had been experiencing a high rate of no-shows for these services before the pandemic. With telehealth, the number of no-shows dropped to almost zero.
In general, telehealth has proved itself worthy of coming out of the prepandemic shadows and becoming a vital component of equitable healthcare.
“I’m happy by how many video visits are still going on,” Millen said. “I was thinking it would fall off rather quickly. But there are certain doctors who really love it and certain patients who really love it.
“I see it getting a little more mature. What’s happened in the last few months is that we’ve created more of a system for it that makes sense. On both sides, I think we all know when to hold it and when to fold it.”
She laughed.
“I mean, when to see them and when to video.”
Wood is a freelance writer.
Get Essential San Diego, weekday mornings
Get top headlines from the Union-Tribune in your inbox weekday mornings, including top news, local, sports, business, entertainment and opinion.
You may occasionally receive promotional content from the San Diego Union-Tribune.





