Does Colon Hydrotherapy Work? Behind the Risks vs. Benefits
Colon Hydrotherapy: What It Is, and When (and If) You Should Use It
- About Colon Hydrotherapy|
- Does Colon Hydrotherapy Work?|
- Alternative Treatments|
- Potential Risks|
- Recommended Products|
As alternative medicine becomes more popular, we’re seeing an influx of promising therapies that could replace or integrate with conventional treatments. Unfortunately, not all of these therapies hold up to their claims.
If you’ve been considering colon hydrotherapy to improve gut health and remove waste from your body, you may want to think twice. Although there’s a potential for short-term benefits, the research unfortunately doesn’t hold up to most of the beneficial claims.
In this article, we’ll discuss what colon hydrotherapy is, the claimed benefits, and the reason why colon cleansing might be more of a band-aid as opposed to an effective remedy for digestive issues.
We’ll then talk about some alternative treatments that have been proven effective, including diet, digestive support, and supplements. These methods can help you get to the root of your digestive issues and promote overall health and well-being.
What Is Colon Hydrotherapy?
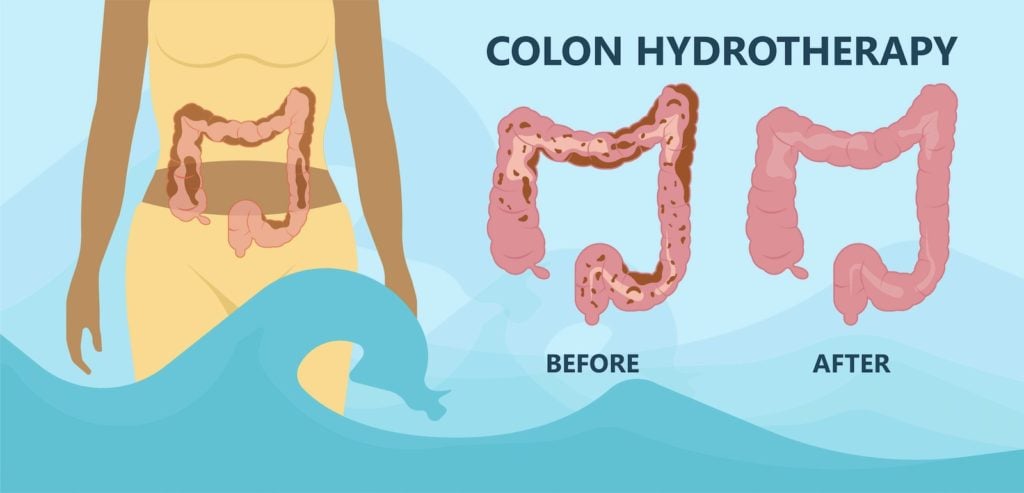
Colon hydrotherapy, also known as a colonic irrigation or colon cleanse, has become increasingly popular over the last 10 years as a way to detox the colon and promote digestive health. People may seek out colon hydrotherapy to assist with removing waste from their large intestine, hoping that it will help with digestive issues like constipation, parasites, or dysbiosis (imbalanced microbiome).
During a colon hydrotherapy session, a tube is inserted into your rectum and large amounts of water (up to 60 liters) are flushed through your colon [1].
Colon hydrotherapy is often confused with enemas, which also include the introduction of water (or herb-infused liquids) into the rectum. However, there are some considerable differences:
| Colon Hydrotherapy | Enema |
| Water reaches higher into the colon | Water reaches only the lower colon |
| Machine pushes water into the colon | Water pushed forward by gravity alone |
| Must be administered by a trained specialist | Can be performed at home |
| Uses up to 60 liters of water | Uses ¼ – 1 liter of water |
Although most research on enemas indicates that they’re relatively safe, some evidence suggests certain kinds of enemeas like coffee enemas may promote issues like lower abdominal pain and bloody stools [2].
Proponents of colon hydrotherapy claim that flushing out the colon results in the removal of harmful toxins. As a result, you can expect increased energy, enhanced digestion, and an immune system boost.
Does Colon Hydrotherapy Work? What the Research Says
Despite the widespread use and popularity of colon hydrotherapy, there’s currently very little scientific evidence to support its benefits. In fact, in a systematic review, investigators reported that no sound research exists to support the practice of colon cleansing. Furthermore, several case studies have described the adverse effects of colon hydrotherapy [3].
Anecdotally, many people have reported benefits following hydrotherapy. What accounts for this discrepancy between research and personal experience? In part, it may be the placebo effect. The placebo effect is very real and very common. In fact, research has consistently shown that the placebo response rate in clinical trials on IBS is around 40%, or as high as 72% [4].
The placebo effect is not inherently bad: if you feel better, that’s a good thing. But in the case of a treatment like colon hydrotherapy which can be expensive, invasive, and potentially harmful, you’re probably better off exploring treatment options that have been proven to help.
From a functional medicine perspective, there are two primary reasons that colon hydrotherapy likely misses the mark when it comes to issues like constipation, dysbiosis, and parasites.

First, colon cleansing doesn’t have any impact on your small intestine. When considering digestive issues, you must take your entire digestive system into account. Nothing in your body happens in a vacuum, and this is especially true when it comes to the gastrointestinal system.
Your stomach, small intestine, and colon all have their separate functions and duties, but they rely on one another to perform their given tasks. By addressing only the colon, you overlook potential imbalances in other parts of your digestive tract.
Second, colon cleansing may provide some short-term relief, but it doesn’t get to the root of your digestive issues. Generally speaking, you shouldn’t “need” colon hydrotherapy. It’s most likely that something else is going on in your digestive tract that’s more deeply rooted. We’ll explore some of these potential root causes, including SIBO and motility issues, below.
Potential Causes of Gut Health Imbalances

Dysbiosis and other imbalances in the gut can lead to all kinds of digestive disturbances, which require a dietary overhaul and thoughtful reintroduction of bacteria instead of flushing out the system.
- SIBO (small intestinal bacterial overgrowth) — SIBO is a condition in which bacteria from other parts of your digestive tract start inhabiting your small intestine. Constipation is a very common symptom of SIBO, along with diarrhea. Some research also suggests a connection between SIBO and irritable bowel disease (IBD) [5].
- Motility issues or scarring — Structural issues or scarring in your digestive tract can make it difficult to pass stools. The cause of these obstructions is typically due to intestinal surgery, where scar tissue builds up and leads to an intestinal blockage [6].
- Dysbiosis — Dysbiosis is a term used to describe gut bacteria that are out of balance, which may involve an increase in the growth of harmful bacteria. As a result, untreated dysbiosis may lead to intestinal permeability, irritable bowel syndrome (IBS), and IBD, all of which may cause inflammation and digestive disturbances [7].
Alternative Treatments to Support Gut Health
Luckily, there are plenty of strategies that can help you get to the root of your digestive issues that are less invasive and much more thorough than colon hydrotherapy.
Diet

When addressing any issue involving gut health, whether it be constipation, dysbiosis, or parasites, your first step should always include looking at your diet. Creating a healthy gut environment is a foundational step in gut healing. You can add in all the therapies you like, but if your gut isn’t optimized for healthy bacteria, it may end up being money down the drain.
The food you eat sets the stage for gut health and can play a pivotal role in whether your gut is inflamed or calm.
For example:
- The Paleo diet helps to reduce inflammation, balance blood sugar, and eliminate common problem foods, all of which can help to support digestive health [8, 9, 10].
- The low FODMAP diet has been shown to improve digestive symptoms associated with SIBO, IBS, and IBD, including gas, abdominal pain, constipation, and bloating [11, 12, 13, 14].
- Avoiding gluten may improve constipation, diarrea, gas, and bloating for those who are sensitive to it [15].
Everyone’s body is different, and therefore everyone’s ideal diet will be unique to them. With that being said, a great place to start is with an elimination diet based on a Paleo framework, which excludes common allergens and inflammatory foods like gluten, dairy, sugar, soy, and processed foods. Based on how you respond to dietary changes, you can begin to reintroduce healthy foods one at a time to see what your body can tolerate, or move on to a more specialized diet if your symptoms have not improved.
Probiotics

Dysbiosis is incredibly common and may result in a host of digestive issues. If cleaning up your diet isn’t enough to shift your gut bacteria back into homeostasis, you may need to include probiotics.
There’s an impressive amount of research behind the positive impact that probiotics can have on improving bowel movements. Specifically, adding probiotics to your regimen may
- Help with stool frequency [16, 17, 18]
- Increase intestinal transit time [16, 17, 18]
- Improve stool consistency [17]
- Reduce bloating [17]
If parasites are at the root of your digestive issues, research shows that Saccharomyces boulardii, a beneficial yeast, may be even more effective than standard antiparasitic drugs [19, 20].
Enzymes and HCl
If you’re low in digestive enzymes or hydrochloric acid (HCl), digestive issues are almost a guarantee.
Digestive enzymes can be very helpful if you have specific food intolerances, as they assist in the breakdown of fat, protein, and carbohydrates. Furthermore, some research shows that digestive enzymes can help IBS (irritable bowel syndrome) symptoms like constipation and diarrhea [21].
Your stomach releases HCl (stomach acid) to help break down proteins, absorb minerals, and control bacteria, parasites, and fungi that may be present in your food. As you age, stomach acid can naturally decrease, but other conditions like autoimmune disease, H. pylori, chronic use of antacids or proton pump inhibitors, and anemia may also contribute to low stomach acid [22, 23, 24].
You can test your need for HCl by slowly incorporating supplements before your meals and assessing how you feel. If you notice burning or any other side effects, either cut back or discontinue the use of HCl.
Antimicrobials

If you’re dealing with a stubborn imbalance of gut bacteria, diet and gut-supportive supplements may not be enough. This is where herbal antimicrobials come in handy. Antimicrobial herbs contain compounds that remove harmful pathogens and make way for the growth of beneficial bacteria [25, 26].
It’s important to note that jumping right into antimicrobials without first addressing your gut environment with diet and lifestyle will do you very little good. Antimicrobials will work to kill off harmful bacteria, but if you’re still inflamed or have suboptimal digestive juices flowing, the harmful bacteria will have fertile ground to replenish themselves.
If, however, you’ve taken the necessary steps to set up your gut environment for success, herbal antimicrobials can do an excellent job of clearing out unwanted pathogens like fungi, bacteria, and parasites [27].
Potential Risks of Colon Hydrotherapy
Unfortunately, in addition to a lack of research supporting its benefits, colon hydrotherapy may come with some potential (although rare) risks.
According to a 2011 literature review, in rare cases colon cleansing may increase risk of [1]:
- Electrolyte imbalance
- Kidney failure
- Liver toxicity
- Rectal perforations
- Perianal gangrene
- Abdominal pain
- Cramping
- Acute water intoxication
- Death from amoeba infections
In another literature review, transanal irrigation (a technique similar to colon hydrotherapy) was found to potentially worsen the following conditions [28]:
- Anal or rectal stenosis (narrowing)
- Active IBD, such as Crohn’s disease
- Acute diverticulitis (small, inflamed pouches that form in your colon)
- Colorectal cancer (colon cancer)
- Rectal surgery within past three months
- Endoscopic polypectomy (minimally invasive polyp removal) within the past four weeks
- Ischemic colitis (inflammation causing too little blood flow to the colon)
Bowel cleansing, in general, may also have detrimental effects on your gut bacteria balance. A randomized controlled trial found that when participants took purgatives (colon cleansing products taken orally), it decreased their total microbial load 31-fold, a drastic reduction in bacteria that could lead to dysbiosis (the growth of harmful bacteria).
While bacterial levels and diversity were restored within 14 days, this is still an unsettling loss of bacteria in a short amount of time. If such colon cleanse products can have such a significant impact on your microbiome, colonic hydrotherapy could potentially produce detrimental effects on colon health [29].
Colon Hydrotherapy: The Takeaway
When considering any imbalance, digestive or otherwise, it’s important to view it from a root cause perspective. Endless therapies claim to be the one-size-fits-all approach to healing, but very few hold up to the hype.
Colon hydrotherapy may offer short-term relief disguised as healing, but both research and reason suggest otherwise.
If you’ve been considering colon hydrotherapy as a way to enhance gut health and promote detoxification, a better option may be to begin with more science-backed holistic strategies that address your root digestive issues.
Begin with diet and lifestyle, and when appropriate, introduce targeted supplements that enhance digestion and kill off harmful bacteria. This approach can help you get to the root of your digestive health problems, while providing other health benefits that support overall wellness.
For step-by-step guidance on reclaiming your gut health, check out my book Healthy Gut, Healthy You. In this book, I detail the steps you need to take to identify the root of your health issues, and gently nudge your body back into balance.
For an even more personalized approach, make an appointment with myself or one of my clinical team members.
Dr. Michael Ruscio is a DC, Naturopathic Practitioner, researcher, and clinician. He serves as an Adjunct Professor at the University of Bridgeport and has published numerous papers in scientific journals as well as the book Healthy Gut, Healthy You. He also founded the Ruscio Institute of Functional Health, where he helps patients with a wide range of GI conditions and serves as the Head of Research.➕ References
- Mishori R, Otubu A, Jones AA. The dangers of colon cleansing. J Fam Pract. 2011 Aug;60(8):454–7. PMID: 21814639.
- Son H, Song HJ, Seo H-J, Lee H, Choi SM, Lee S. The safety and effectiveness of self-administered coffee enema: A systematic review of case reports. Medicine (Baltimore). 2020 Sep 4;99(36):e21998. DOI: 10.1097/MD.0000000000021998. PMID: 32899046. PMCID: PMC7478478.
- Acosta RD, Cash BD. Clinical effects of colonic cleansing for general health promotion: a systematic review. Am J Gastroenterol. 2009 Nov;104(11):2830–6; quiz 2837. DOI: 10.1038/ajg.2009.494. PMID: 19724266.
- Ballou S, Beath A, Kaptchuk TJ, Hirsch W, Sommers T, Nee J, et al. Factors associated with response to placebo in patients with irritable bowel syndrome and constipation. Clin Gastroenterol Hepatol. 2018 Nov;16(11):1738-1744.e1. DOI: 10.1016/j.cgh.2018.04.009. PMID: 29654913. PMCID: PMC6414074.
- Dukowicz AC, Lacy BE, Levine GM. Small intestinal bacterial overgrowth: a comprehensive review. Gastroenterol Hepatol (N Y). 2007 Feb;3(2):112–22. PMID: 21960820. PMCID: PMC3099351.
- Abdominal Adhesions | NIDDK [Internet]. [cited 2021 Jul 11]. Available from: https://www.niddk.nih.gov/health-information/digestive-diseases/abdominal-adhesions#what
- Belizário JE, Faintuch J. Microbiome and gut dysbiosis. Exp Suppl. 2018;109:459–76. DOI: 10.1007/978-3-319-74932-7_13. PMID: 30535609.
- Whalen KA, McCullough ML, Flanders WD, Hartman TJ, Judd S, Bostick RM. Paleolithic and Mediterranean Diet Pattern Scores Are Inversely Associated with Biomarkers of Inflammation and Oxidative Balance in Adults. J Nutr. 2016 Jun;146(6):1217–26. DOI: 10.3945/jn.115.224048. PMID: 27099230. PMCID: PMC4877627.
- Olendzki BC, Silverstein TD, Persuitte GM, Ma Y, Baldwin KR, Cave D. An anti-inflammatory diet as treatment for inflammatory bowel disease: a case series report. Nutr J. 2014 Jan 16;13:5. DOI: 10.1186/1475-2891-13-5. PMID: 24428901. PMCID: PMC3896778.
- Masharani U, Sherchan P, Schloetter M, Stratford S, Xiao A, Sebastian A, et al. Metabolic and physiologic effects from consuming a hunter-gatherer (Paleolithic)-type diet in type 2 diabetes. Eur J Clin Nutr. 2015 Aug;69(8):944–8. DOI: 10.1038/ejcn.2015.39. PMID: 25828624.
- Marsh A, Eslick EM, Eslick GD. Does a diet low in FODMAPs reduce symptoms associated with functional gastrointestinal disorders? A comprehensive systematic review and meta-analysis. Eur J Nutr. 2016 Apr;55(3):897–906. DOI: 10.1007/s00394-015-0922-1. PMID: 25982757.
- Gibson PR, Shepherd SJ. Food choice as a key management strategy for functional gastrointestinal symptoms. Am J Gastroenterol. 2012 May;107(5):657–66; quiz 667. DOI: 10.1038/ajg.2012.49. PMID: 22488077.
- Altobelli E, Del Negro V, Angeletti PM, Latella G. Low-FODMAP Diet Improves Irritable Bowel Syndrome Symptoms: A Meta-Analysis. Nutrients. 2017 Aug 26;9(9). DOI: 10.3390/nu9090940. PMID: 28846594. PMCID: PMC5622700.
- Gibson PR, Shepherd SJ. Evidence-based dietary management of functional gastrointestinal symptoms: The FODMAP approach. J Gastroenterol Hepatol. 2010 Feb;25(2):252–8. DOI: 10.1111/j.1440-1746.2009.06149.x. PMID: 20136989.
- Volta U, Bardella MT, Calabrò A, Troncone R, Corazza GR, Study Group for Non-Celiac Gluten Sensitivity. An Italian prospective multicenter survey on patients suspected of having non-celiac gluten sensitivity. BMC Med. 2014 May 23;12(1):85. DOI: 10.1186/1741-7015-12-85. PMID: 24885375. PMCID: PMC4053283.
- Wen Y, Li J, Long Q, Yue C-C, He B, Tang X-G. The efficacy and safety of probiotics for patients with constipation-predominant irritable bowel syndrome: A systematic review and meta-analysis based on seventeen randomized controlled trials. Int J Surg. 2020 Jul;79:111–9. DOI: 10.1016/j.ijsu.2020.04.063. PMID: 32387213.
- Zhang C, Jiang J, Tian F, Zhao J, Zhang H, Zhai Q, et al. Meta-analysis of randomized controlled trials of the effects of probiotics on functional constipation in adults. Clin Nutr. 2020 Oct;39(10):2960–9. DOI: 10.1016/j.clnu.2020.01.005. PMID: 32005532.
- Miller LE, Ouwehand AC, Ibarra A. Effects of probiotic-containing products on stool frequency and intestinal transit in constipated adults: systematic review and meta-analysis of randomized controlled trials. Ann Gastroenterol. 2017 Sep 21;30(6):629–39. DOI: 10.20524/aog.2017.0192. PMID: 29118557. PMCID: PMC5670282.
- Dinleyici EC, Eren M, Dogan N, Reyhanioglu S, Yargic ZA, Vandenplas Y. Clinical efficacy of Saccharomyces boulardii or metronidazole in symptomatic children with Blastocystis hominis infection. Parasitol Res. 2011 Mar;108(3):541–5. DOI: 10.1007/s00436-010-2095-4. PMID: 20922415.
- Besirbellioglu BA, Ulcay A, Can M, Erdem H, Tanyuksel M, Avci IY, et al. Saccharomyces boulardii and infection due to Giardia lamblia. Scand J Infect Dis. 2006;38(6–7):479–81. DOI: 10.1080/00365540600561769. PMID: 16798698.
- Weir I, Shu Q, Wei N, Wei C, Zhu Y. Efficacy of actinidin-containing kiwifruit extract Zyactinase on constipation: a randomised double-blinded placebo-controlled clinical trial. Asia Pac J Clin Nutr. 2018;27(3):564–71. DOI: 10.6133/apjcn.122017.03. PMID: 29737803.
- Betesh AL, Santa Ana CA, Cole JA, Fordtran JS. Is achlorhydria a cause of iron deficiency anemia? Am J Clin Nutr. 2015 Jul;102(1):9–19. DOI: 10.3945/ajcn.114.097394. PMID: 25994564.
- Proton Pump Inhibitors – What Are PPIs & How Do PPIs Work? [Internet]. [cited 2021 Jul 8]. Available from: https://www.drugwatch.com/proton-pump-inhibitors/
- Guilliams TG, Drake LE. Meal-Time Supplementation with Betaine HCl for Functional Hypochlorhydria: What is the Evidence? Integr Med (Encinitas). 2020 Feb;19(1):32–6. PMID: 32549862. PMCID: PMC7238915.
- Chen C, Tao C, Liu Z, Lu M, Pan Q, Zheng L, et al. A Randomized Clinical Trial of Berberine Hydrochloride in Patients with Diarrhea-Predominant Irritable Bowel Syndrome. Phytother Res. 2015 Nov;29(11):1822–7. DOI: 10.1002/ptr.5475. PMID: 26400188.
- Chedid V, Dhalla S, Clarke JO, Roland BC, Dunbar KB, Koh J, et al. Herbal therapy is equivalent to rifaximin for the treatment of small intestinal bacterial overgrowth. Glob Adv Health Med. 2014 May;3(3):16–24. DOI: 10.7453/gahmj.2014.019. PMID: 24891990. PMCID: PMC4030608.
- Wink M. Medicinal plants: a source of anti-parasitic secondary metabolites. Molecules. 2012 Oct 31;17(11):12771–91. DOI: 10.3390/molecules171112771. PMID: 23114614. PMCID: PMC6268567.
- Emmanuel AV, Krogh K, Bazzocchi G, Leroi AM, Bremers A, Leder D, et al. Consensus review of best practice of transanal irrigation in adults. Spinal Cord. 2013 Oct;51(10):732–8. DOI: 10.1038/sc.2013.86. PMID: 23958927.
- Jalanka J, Salonen A, Salojärvi J, Ritari J, Immonen O, Marciani L, et al. Effects of bowel cleansing on the intestinal microbiota. Gut. 2015 Oct;64(10):1562–8. DOI: 10.1136/gutjnl-2014-307240. PMID: 25527456.




Discussion
I care about answering your questions and sharing my knowledge with you. Leave a comment or connect with me on social media asking any health question you may have and I just might incorporate it into our next listener questions podcast episode just for you!