I’m Treating Too Many Young People for the Coronavirus
Americans in their 20s and 30s—no matter how healthy and invincible they feel—need to understand how dangerous this virus can be.
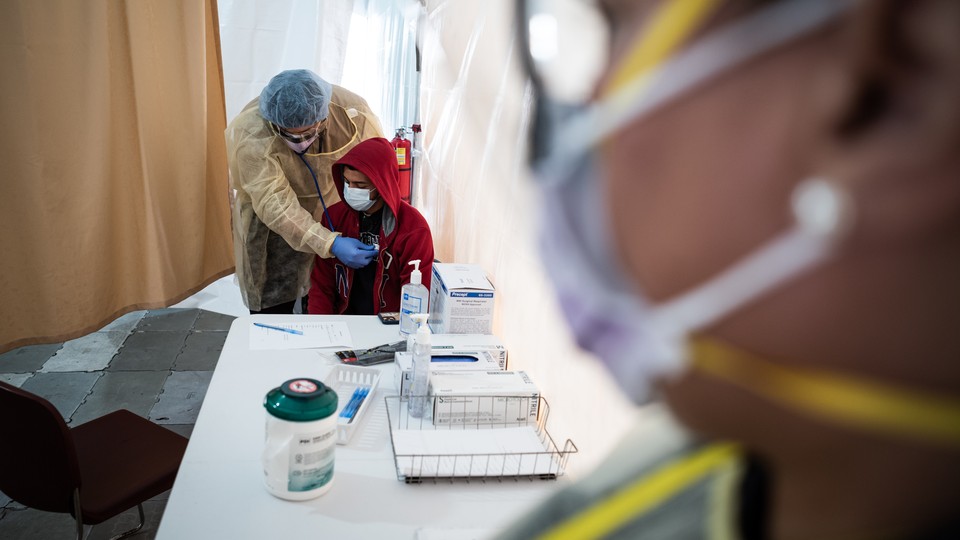
On Friday night, I worked a 12-hour shift in the designated COVID-19 area of my hospital’s emergency department in New York City. Over the course of the night, I examined six patients who were exhibiting common symptoms of the novel coronavirus; five of them were in their 20s or early 30s.
I am 28 years old. Up until Friday, when people asked me whether I was scared, I would tell them yes—for my country, my colleagues, my 92-year-old grandmother, and all the people most vulnerable to getting seriously ill from the virus, but not for myself. I, like many others, believed that young people were less likely to get sick, and that if they did, the illness was mild, with a quick recovery.
I now know that isn’t the case. The fact is that young people with no clear underlying health conditions are getting seriously ill from COVID-19 in significant numbers. And young Americans—no matter how healthy and invincible they feel—need to understand that.
My first patient was in their early 20s. (To protect their confidentiality, I’m referring to my patients without mentioning their gender.) They had a dry cough and a 102-degree fever, but their chest X-ray came back clear and their oxygen levels were safe. I wanted to test them for COVID-19, but they weren’t sick enough to require admission to the hospital, which meant I couldn’t do so. We desperately want to be able to test and take care of everyone, from the seriously ill to the mildly sick and worried, but with our current capacity, we simply can’t. I told them that they needed to assume they had the virus, and gave them instructions on how to quarantine at home.
I changed my gown and gloves, checked my mask and goggles, and moved on to my next patient: a student who had been coughing and feeling fatigued for multiple days. They had been with a friend before getting sick, and that friend had since fallen ill with symptoms of COVID-19, including a fever. The patient was having trouble catching their breath, but their symptoms were not severe or acute—as confirmed by a chest X-ray and a test of their oxygen levels—so I recommended discharge and quarantine, and they understood.
My next patient was a young professional. For the past week they’d had a dry cough and chest pain. They had no underlying health conditions, and they’d tried to follow the current guidelines by staying at home (the right thing to do, given the overwhelmed state of hospitals like mine) but that evening their breathing had become so labored that they called an ambulance. When I saw them, however, they were breathing comfortably, their chest X-ray was clear, and their oxygen levels were safe. They were visibly upset when I told them they would not be admitted. They wanted to be tested. I explained why we couldn’t do that, and completed their discharge paperwork.
I collected myself and approached my next patient: a young person who’d been suffering with a fever, cough, and extreme fatigue for the past three days. Their boss didn’t believe they were sick, so they’d continued to complete long shifts working with customers at a local business. After examining the young patient, I determined that they were in the same category as the previous three I’d seen—sick, but not sick enough to be given a precious hospital bed or COVID-19 test—so I gave them fluids, Tylenol, and a note for their employer confirming that they were indeed ill, and needed to stay home.
Late in the night, another young patient came in with a high fever and no underlying health conditions. They’d had a dry cough for the past four days. They’d come to the hospital after finding they were unable to walk a few feet without getting severely short of breath. On their chest X-ray, I saw lungs that were almost completely whited out, indicating a significant amount of inflammation. It was clear how uncomfortable they were, and how desperately they were trying to catch their breath. They were in a different category from the previous patients I’d seen that night. They needed to be admitted. They needed testing. They needed close monitoring.
I called the Intensive Care Unit team, and they admitted the young patient to the hospital. I finished my shift not long after, walked home, and got in bed, feeling unsteady. When I woke up a few hours later, I logged into our electronic medical record system and learned that in the time I’d been asleep, my patient’s oxygen levels had dropped severely. A breathing tube had been placed down their throat. A ventilator was now keeping them alive.
Recent statistics suggest that what I saw that night is not unusual. On Tuesday, California Governor Gavin Newsom said that half of the 2,102 people who had tested positive for COVID-19 in his state were ages 18 to 49. The Centers for Disease Control and Prevention published data on March 18 showing that, from February 12 to March 16, nearly 40 percent of American COVID-19 patients who were sick enough to be hospitalized were ages 20 to 54. Twelve percent of patients with the most critical cases, requiring admission to an ICU, were ages 20 to 44. There are some caveats worth noting: The CDC was not able to determine whether the young people included in its report had underlying health conditions. And all of this is early data. We know that we are still not testing nearly enough people in the United States. The numbers may change.
But in spite of these alarming figures, too many young Americans have been slow to give up the false belief that they are safe from COVID-19. The day after the CDC report was released, college students began responding to a poll. Only 50 percent said that they were concerned about contracting COVID-19. Fifty-three percent admitted that they or their friends had gone to social gatherings in the previous week.
At the same time as I was seeing the flurry of young patients on my overnight shift, a resident friend of mine at a hospital on the West Coast was placing a patient in their 20s on a ventilator. A 26-year-old woman who was hospitalized with COVID-19 recently told her story in The New York Times. A doctor at my own hospital said that he has never seen so many young people in the ICU as he’s now seeing with COVID-19.
This isn’t the type of evidence that we like to talk about as scientists—anecdotes, instead of hard data—but doctors are people too. We listen to the stories of our patients and our colleagues. We pay attention to the trends that we see on the ground. We connect the dots.
We still need better data to fully understand how young people are being affected by COVID-19, but until we can get it, we have to spread the word, and ask friends and family—no matter their age—to stay at home.