Long Covid
My Son’s Crushing Long-COVID Journey
Personal Perspective: False assumptions made it hard to find care.
Updated March 12, 2024 Reviewed by Michelle Quirk
Key points
- Long COVID is a complex condition that can affect kids' quality of life.
- Families need more support and recognition from medical professionals.
- Fatigue and brain fog aren't a frame of mind for long-COVID patients. They are physiological functions.

School had started, but my 11-year-old son Marty was in bed. His backpack leaned against the wall. It was a relic, filled with barely touched 6th-grade textbooks and colored folders in plastic wrap.
“You’ve got to get up,” I said. “You’re missing so much.”
“I’m too tired.”
The first week of middle school, Marty caught COVID-19. He had a fever, sore throat, and a cough. After 10 days, he tested negative. But when it was time to get moving, he was listless.
“My body feels heavy,” he said. “I can’t think straight.”
While his classmates divided fractions and made friends, Marty was home with intermittent fevers, abdominal cramping, and massive fatigue.
I took him to the pediatrician, who ran blood tests and checked his vital signs.
“Could it be long COVID?” I asked. The doctor gazed at me like I said hocus pocus.
“Everything looks normal,” he said.
But my kid couldn’t function.
Could Long COVID Be a Choice?
After a month, Marty had lost 10 pounds and all his energy. Before a walk around the block, he rested at the front door. He couldn’t pick up a pencil, much less make his way around a new school. I told an administrator that Marty wouldn’t be coming to class.
“Maybe it’s school refusal,” she said and suggested counseling.
Every day was a sick day that left me scrambling. Marty went from being fully functional to needing 24-7 help, and motherhood felt like an alien experience.
At social events, moms shared stories about their kids’ busy schedules, basketball games, and new friend groups, but my mind was on Marty’s medical records, inflammatory molecules, and post-exertional malaise.
“Marty is always exhausted,” I said to another mom.
“My kids get tired, but they push through,” she replied. “It must be psychological.”
Sometimes it seemed that way. Occasionally Marty visited friends or took short walks. But after any activity he crashed.
“Put mind over matter!” I said.
Little did I know that microscopic particles were robbing his body of the ability to produce power.
When an Illness Isn’t Accepted
Time stood still. As his friends built their muscles and brains, Marty’s life atrophied. I felt desperate. It wasn’t the first time a chronic condition crushed him.
As I wrote in this post, Marty had suffered from undiagnosed celiac disease, a gut disorder that wreaked havoc on his brain. He was catching up on years of lost learning when COVID-19 hit.
I saw his condition as a crime scene. Something hijacked his quality of life, and I wanted to find out whodunnit. I made appointments with five specialists who couldn’t figure it out.
“There’s no inflammation. His immune system is fine.”
“Brain fog isn’t a medical condition. He can get to school.”
“His symptoms aren’t related to COVID. It’s something else.”
I got the message that my parenting stinks. Maybe it does. But that’s not what caused Marty’s malaise.
“There’s no mystery here. COVID can infect almost every cell type in the human body [and] every organ, the brain, and the central nervous system,” said Amy Proal, a microbiologist who is the president of the PolyBio Research Foundation and director of its Long COVID Research Consortium.
Proal’s research shows that viral remnants from COVID-19 can remain in the body, triggering inflammation and causing symptoms that include fatigue and cognitive clouding. But that information hasn’t made its way to enough frontline physicians. “There’s a gap in understanding that pathogens can drive many chronic problems. It’s a gap in education [that] should be filled by logic,” she said.
The system has blind spots. General practice doctors like pediatricians aren’t typically trained to treat or diagnose complex, multisystem symptoms. And specialists often function in strict silos, missing the big picture, according to three medical researchers and clinicians.
When There’s Nowhere Else to Turn
I hit a wall. And I wasn’t alone. Thousands of parents struggle to find help for their kids with long COVID. Some join online communities where they share research studies, treatment options, and personal stories.
“Long COVID has gutted every aspect of our lives in the last two years,” said Jennifer, a mom who is part of a support group.
Her son Fergus developed fevers, chest pain, and vocal and motor tics after multiple cases of COVID-19, but doctors didn’t consider the virus a possible cause. She turned to Facebook to get information and tracked down a specialist who diagnosed her son with a tic disorder due to COVID-19 a year later.
“Why aren’t doctors keeping up with research?” she said. “It feels irresponsible that I am looking for help on Facebook. It shouldn’t be this way."
But that’s the reality for many moms.
“Kids come to our Long COVID clinic who have been dismissed as being lazy or choosing school avoidance. It’s not the case,” said Alexandra Yonts, an infectious disease doctor and the director of the post-COVID pediatric program at the Children’s National Hospital in Washington, D.C.
“Fatigue is the most common symptom. I have pediatric patients who sleep 20 hours a day,” she said. “This population group is really suffering.”
Long COVID is complicated, especially in kids, who can’t always explain their condition. Estimates vary, but a systematic review in Pediatrics found that one out of six kids will experience lingering, post-COVID symptoms. And the medical system isn’t set up to support them.
Healing Is More Than a Cure
To help Marty, I took a DIY approach. When the sun went down, I went to work. With Dr. Google’s guidance, I got a virtual Ph.D. on cytokines, T-cells, and pathophysiology.
I searched for the best sources and found David Putrino, a neuroscientist whose research suggests that systemic inflammation after COVID-19 can cause a range of symptoms. He runs a rehabilitation lab at Mt. Sinai Hospital, just blocks from my apartment. I emailed him and he responded right away.
“I’d like to help,” he said. “Let’s take a deeper dive and see what we discover.”
For the first time in months, I exhaled.
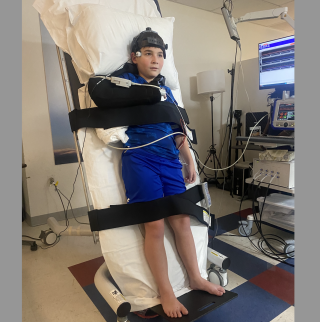
Marty and I found our way to a space filled with machines that made me think of Dr. Frankenstein’s laboratory. “This lab is cool!” Marty said.
A technician chatted with Marty about Fortnite skins, Roblox games, and brain fog.
Marty extended his arm for a blood test that checked for clotting. He spent an hour strapped to a tilt table with electrodes attached to his head and legs that assessed his autonomic nervous system. The results gave us great intel.
“There are microclots in Marty’s blood,” Putrino said. “That could cause fatigue and brain fog.”
In some long COVID patients, researchers discovered tiny clots made of proteins and inflammatory molecules that can damage the cells that line blood vessels and reduce the amount of oxygen that gets to vital organs, including the brain.
That's one reason Marty was wiped out. He also has a blood pressure problem that long COVID can cause.
The damage was there, but it didn’t show up in typical tests.
Seeing My Son’s Strength
It has been four months since Marty developed long COVID. I consider him lucky. He has health insurance and parents who can fit work calls in between doctor visits. Most importantly, he found the right support.

Each morning, Marty takes supplements and medicine that help his vascular, immune, and digestive systems. He works with a specialized physical therapist. He’s well enough to learn at home a few hours a day.
I’m grateful for his progress. But more than anything, understanding the science behind long COVID gave me more than tangible data.
“It’s time to get up,” I said the other morning. “The math teacher is here.”
“I need more time,” Marty said. “I’m lazy.”
“No, you’re lethargic because you have tiny blobs in your blood that make you feel extra tired,” I said. “You’re a fighter, and I’m proud of you.”
Now I can set the record straight.
Tips for Finding Support
- Consider a school plan. If your child is unable to get to school, ask the doctor for help implementing a 504 plan, which ensures that a child with a disability receives accommodations that could include extra time for tests and excused medical absences.
- Don’t overdo it. Lindsay McAlpine, a neurologist who directs Yale’s NeuroCOVID Clinic, said people with long COVID can become disabled in two weeks. Research shows damage in their muscles, indicating a depleted ability to function. “I have to untrain people and give them permission to back off,” she said. She recommends a gradual approach to recovery.
- Believe in biology. If doctors dismiss mood-related symptoms, ask them to suggest specialists who might be able to access micro-clot testing and autonomic nervous system assessments, two potential markers for a long COVID diagnosis.
References
Liji Thomas. New research finds microclotting and inflammatory molecule abnormalities in long-COVID. News-Medical.Net. October 18, 2022.
Sara Reardon. Blood Clotting Proteins Might Help Predict Long COVID Brain Fog. Scientific American. September 1, 2023.




