Abstract
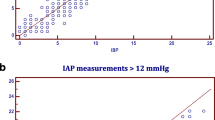
Increased intra-abdominal pressure (IAP) is an important vital sign in critically ill patients and has a negative impact on morbidity and mortality. This study aimed to validate a novel non-invasive ultrasonographic approach to IAP measurement against the gold standard intra-bladder pressure (IBP) method. We conducted a prospective observational study in an adult medical ICU of a university hospital. IAP measurements using ultrasonography by two independent operators, with different experience levels (experienced, IAPUS1; inexperienced, IAPUS2), were compared with the gold standard IBP method performed by a third blinded operator. For the ultrasonographic method, decremental external pressure was applied on the anterior abdominal wall using a bottle filled with decreasing volumes of water. Ultrasonography looked at peritoneal rebound upon brisk withdrawal of the external pressure. The loss of peritoneal rebound was identified as the point where IAP was equal to or above the applied external pressure. Twenty-one patients underwent 74 IAP readings (range 2–15 mmHg). The number of readings per patient was 3.5 ± 2.5, and the abdominal wall thickness was 24.6 ± 13.1 mm. Bland and Altman’s analysis showed a bias (0.39 and 0.61 mmHg) and precision (1.38 and 1.51 mmHg) for the comparison of IAPUS1 and IAPUS2 and vs. IBP, respectively with small limits of agreement that were in line with the research guidelines of the Abdominal Compartment Society (WSACS). Our novel ultrasound-based IAP method displayed good correlation and agreement between IAP and IBP at levels up to 15 mmHg and is an excellent solution for quick decision-making in critically ill patients.




Similar content being viewed by others
Data Availability
Derived data supporting the findings of this study in addition to the processing algorithms are available from the corresponding author on request.
References
Carter BM, Howard C. A 6th vital sign–potential use of nasogastric tube for intra-abdominal pressure monitoring method to detect feeding intolerance in very low birth-weight Preterm Infants (< 1500 g). Adv Neonatal Care. 2015;15(3):176–81.
Kirkpatrick AW, et al. WSACS–The Abdominal Compartment Society. A Society dedicated to the study of the physiology and pathophysiology of the abdominal compartment and its interactions with all organ systems. Anaesthesiol Intensive Ther. 2015;47(3):191–4.
Kirkpatrick AW, et al. Update from the Abdominal Compartment Society (WSACS) on intra-abdominal hypertension and abdominal compartment syndrome: past, present, and future beyond Banff 2017. Anaesthesiol Intensive Ther. 2017;49(2):83–7.
Sugrue M, et al. Clinical examination is an inaccurate predictor of intraabdominal pressure. World J Surg. 2002;26(12):1428–31.
Jacobs R et al. Fluid Management, Intra-Abdominal Hypertension and the Abdominal Compartment Syndrome: A Narrative Review. Life (Basel), 2022. 12(9).
Minini A, Emara MM, Malbrain MLNG et al. Polycompartment Syndrome, in Compartment Syndrome, F. Coccolini, Editors. 2021, Springer International Publishing: Cham. p. 101–121.
De Laet I, Hoste E, De Waele JJ. Transvesical intra-abdominal pressure measurement using minimal instillation volumes: how low can we go? Intensive Care Med. 2008;34(4):746–50.
De Waele JJ, et al. The effect of different reference transducer positions on intra-abdominal pressure measurement: a multicenter analysis. Intensive Care Med. 2008;34(7):1299–303.
Al-Hwiesh A, et al. Intraperitoneal pressure and intra-abdominal pressure: are they the same? Perit Dial Int. 2011;31(3):315–9.
Khanna AK, Rola P, Malbrain M. Biomarkers for intra-abdominal pressure: another tool in the toolbox? Eur Heart J Acute Cardiovasc Care. 2022;11(6):461–3.
David M, et al. Intra-abdominal pressure monitoring by Surface Bioimpedance Estimation. J Phys: Conf Ser. 2019;1272(1):012013.
Tang H, et al. Deep Domain Adaptation for Predicting Intra-Abdominal pressure with multichannel attention Fusion Radar Chip. Adv Intell Syst. 2022;4(5):2100209.
Tayebi S, et al. Non-invasive intra-abdominal pressure measurement by means of transient Radar Method: in Vitro Validation of a Novel Radar-Based Sensor. Sensors. 2021;21(18):5999.
David M, et al. Non-invasive indirect monitoring of intra-abdominal pressure using microwave reflectometry: system design and proof-of-concept clinical trial. J Clin Monit Comput. 2021;35(6):1437–43.
Cheatham ML, et al. The impact of body position on intra-abdominal pressure measurement: a multicenter analysis*. Crit Care Med; 2009.
Cheatham ML et al. Results from the International Conference of Experts on Intra-abdominal Hypertension and Abdominal Compartment Syndrome. II. Recommendations Intensive Care Med, 2007. 33(6): p. 951 – 62.
Malbrain ML. Different techniques to measure intra-abdominal pressure (IAP): time for a critical re-appraisal. Intensive Care Med. 2004;30(3):357–71.
Malbrain ML, et al. Prevalence of intra-abdominal hypertension in critically ill patients: a multicentre epidemiological study. Intensive Care Med. 2004;30(5):822–9.
Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986;1(8476):307–10.
Tayebi S et al. Pre-Clinical Validation of A Novel Continuous Intra-Abdominal Pressure Measurement Equipment (SERENNO) Life (Basel), 2022. 12(8).
Otto J, et al. Direct intra-abdominal pressure monitoring via piezoresistive pressure measurement: a technical note. BMC Surg. 2009;9:5.
Malbrain ML, et al. Can the abdominal perimeter be used as an accurate estimation of intra-abdominal pressure? Crit Care Med. 2009;37(1):316–9.
van Ramshorst GH, et al. Non-invasive measurement of intra-abdominal pressure: a preliminary study. Physiol Meas. 2008;29(8):N41–7.
Tayebi S, et al. A concise overview of non-invasive intra-abdominal pressure measurement techniques: from bench to bedside. J Clin Monit Comput. 2021;35(1):51–70.
Acknowledgements
The authors wish to thank the physicians and nurses of the Medical Intensive Care Unit, National University Hospital, Singapore, for their enthusiasm and support for this study. The authors of the ETRO department acknowledge the “SB Ph.D. fellow at FWO” (“SB-doctoraatsbursaal van het FWO”), Fonds Wetenschappelijk Onderzoek—Vlaanderen, Research Foundation—Flanders, project number: 1S51122N. No other (financial) support was provided.
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. The first draft of the manuscript was written by Kay Choong See and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics Approval
The study protocol was approved by the institutional review board of the local ethics committee (study number B/09/032).
Consent to participate
Written informed consent was obtained from all subjects involved in the study.
Competing interests
M.L.N.G.M. is Professor of Critical Care Research at the 1st Department of Anaesthesiology and Intensive Therapy, Medical University of Lublin, Poland. He is co-founder, past-President, and current Treasurer of WSACS (The Abdominal Compartment Society, http://www.wsacs.org). He is member of the medical advisory Board of Pulsion Medical Systems (part of Getinge group), Serenno Medical, Potrero Medical, and Baxter, and consults for BBraun, Becton Dickinson, ConvaTec, Spiegelberg, and Holtech Medical. He received speaker’s fees from PeerVoice. He is co-founder and President of the International Fluid Academy (IFA). The IFA (http://www.fluidacademy.org) is integrated within the not-for-profit charitable organization iMERiT, the International Medical Education and Research Initiative, under Belgian law. The other authors have no potential conflicts of interest in relation to the contents of this paper.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
10877_2023_1024_MOESM1_ESM.wmv
Supplementary Material 1: Online resource 1. Video recording of peritoneal lining when IAP is higher than the external pressure. In this case, no peritoneal rebound can be observed.
10877_2023_1024_MOESM2_ESM.wmv
Supplementary Material 2: Online resource 2. Video recording of the peritoneal lining when IAP is lower than the external pressure. In this situation, peritoneal rebound can be observed immediately after the brisk removal of the external pressure.
10877_2023_1024_MOESM3_ESM.tif
Supplementary Material 3: Online resource 3. Intra-class correlation coefficient (ICC) for intra-bladder pressure (IBP) and IAPus. As can be seen, a relatively high (single and average measures) ICC was observed for the recorded data, which represents the reliability of the measurements.
10877_2023_1024_MOESM4_ESM.tif
Supplementary Material 4: Online resource 4. Bland and Altman?s analysis between results of the experienced (IAPus1) and inexperienced (IAPus2) operators. The small bias (0.23 mmHg) and precision (0.62 mmHg) shows excellent agreement between the measurements by experienced and inexperienced operators.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
See, K.C., Tayebi, S., Sum, C.L. et al. Feasibility analysis of a novel non-invasive ultrasonographic method for the measurement of intra-abdominal pressure in the intensive care unit. J Clin Monit Comput 37, 1351–1359 (2023). https://doi.org/10.1007/s10877-023-01024-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-023-01024-2