The 1918 pandemic mistake that changed medicine forever
A misunderstanding about the microbe that actually causes the flu created a ripple effect that changed the future of U.S. drug development, clinical trials, and pandemic preparedness.
In 1892 a prominent German bacteriologist named Richard Pfeiffer made a mistake—one that would have an enormous impact on the pandemic of 1918 and the next century of medicine.
In the late 19th century scientists had begun to draw connections between microorganisms and human illnesses. But no one had convincingly linked a specific pathogen to influenza, which back then was essentially a catchall term for a suite of infectious respiratory symptoms that had swept through populations for millennia.
To solve the mystery, Pfeiffer was examining sputum from 31 patients who had died in the flu pandemic of 1889-90, which killed about a million people worldwide. That’s when he discovered a new type of bacterium. “The influenza bacilli appear as tiny little rodlets,” he reported in the British Medical Journal in January 1892, and he found them exclusively in pandemic victims. “In view of these results, I consider myself justified in pronouncing the bacilli just described to be the exciting causes of influenza.”
He named the bacterium Bacillus influenzae, but it quickly became known known as Pfeiffer’s bacillus. After all, Pfeiffer was chief of the Scientific Section of the Berlin Institute for Infectious Diseases and a protégé of Robert Koch, a microbiology pioneer. His stature was such that people readily believed him. This was still the case 26 years later, in 1918, when people began dying at alarming rates from an infectious respiratory disease.


We now know that a flu virus, not a bacterium, caused the infamous pandemic. But in 1918 no one knew the flu virus existed. Instead, scientists of the era initially blamed the deadly scourge on Pfeiffer’s bacillus.
Today Pfeiffer’s story is a potent reminder of the challenges scientists face when a novel microscopic threat emerges. Efforts to pin down the connection between the bacterium and the rapidly spreading disease led to many frustrations and setbacks, including multiple failed attempts to develop an effective vaccine. By summer 1919 tens of millions were dead across the globe, and scientists still did not agree on what, exactly, had killed them.
Still, the mistake and its consequences had a lasting effect on science and medicine, ultimately generating new standards for research and drug development, some of which are still in place today. The scientists working during the 1918 pandemic “were very thoughtful, smart, hard-working people, doing their very best, using their knowledge base and their technology,” says Jeffrey Taubenberger, head of viral pathogenesis and evolution at the National Institute of Allergy and Infectious Diseases (NIAID).
The work led to new treatments for other diseases, hastened the formation of national and global public health institutions, and left us better prepared to deal with modern pandemics, including COVID-19.
‘Not quite sure what we know’
Though the disease is erroneously called the Spanish flu, it first appeared at a U.S. Army base in Kansas, where more than 56,000 soldiers were destined for the trenches of World War I. The pathogen quickly spread to other Army camps, and hundreds of thousands of infected soldiers were subsequently shipped across the Atlantic Ocean. By that summer terrible outbreaks were happening around the world.
In September 1918 then-U.S. Surgeon General Rupert Blue issued guidelines for physicians dealing with the pandemic titled: “Infectious agent—the bacillus of Pfeiffer.” That prompted another misstep: Teams across the nation begin concocting vaccines based on the bacterium.

Yet in October 1918 alone, more than 200,000 people in the U.S. died from the mysterious new flu, including scores of vaccine recipients.
To figure out why vaccines were failing to prevent deaths, physicians and pathologists collected samples from the lungs of the living and the dead and analyzed them in their labs. They found teeming colonies of Streptococcus, Pneumococcus, and Staphylococcus aureus bacteria—but much less of Pfeiffer’s bacillus. Confoundingly, they also found Pfeiffer’s bacillus in many healthy people.
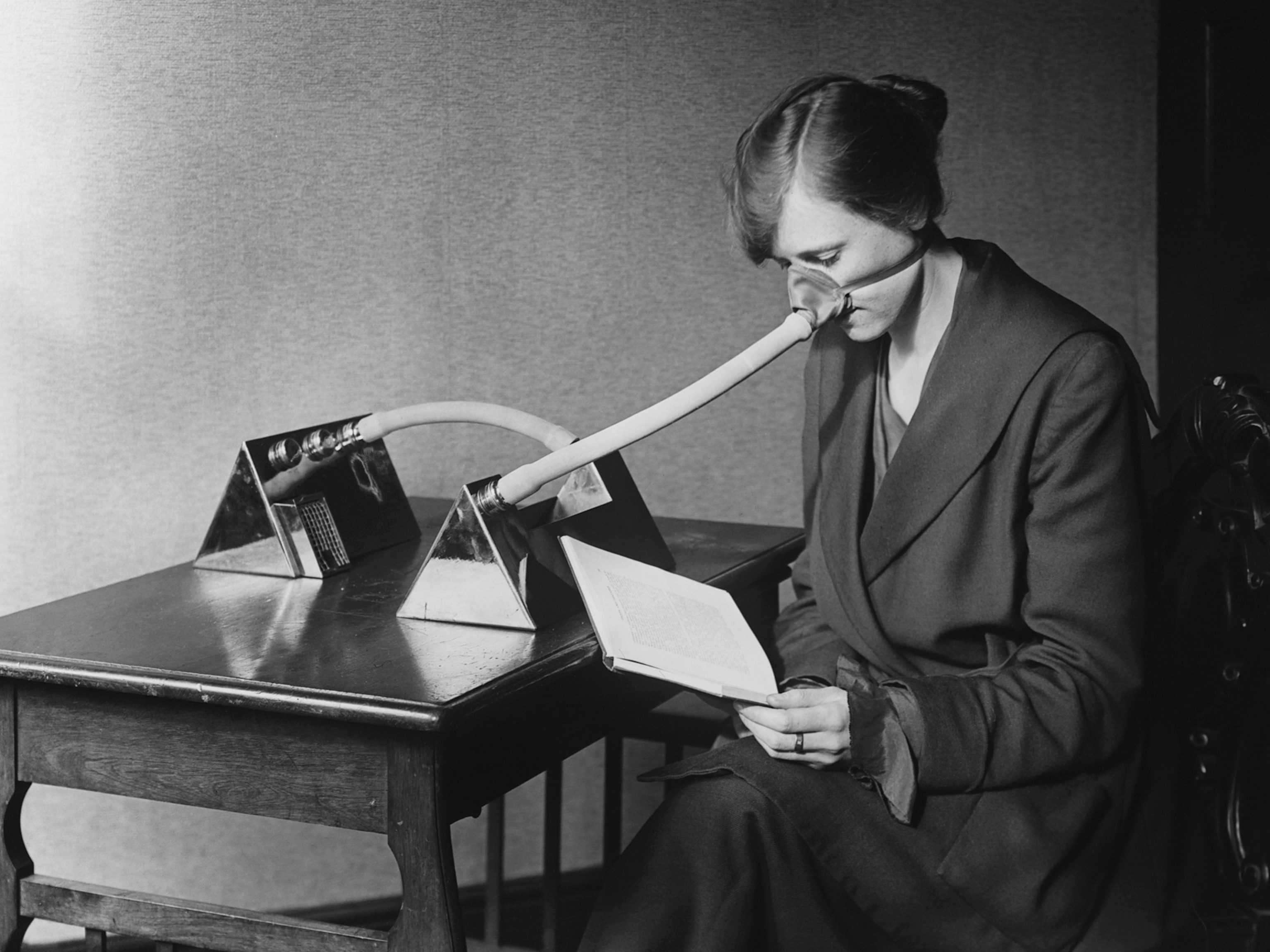
The Public Health Service and the U.S. Navy conducted more audacious experiments on enlisted volunteers in late 1918. The researchers first sprayed a pure culture of Pfeiffer’s bacillus into volunteers’ noses. When none of them got sick, “we became bolder,” prominent public health official Milton Rosenau recounted in an August 1919 publication.
The team had volunteers and influenza patients come together “muzzle to muzzle,” and the ill patients exhaled into the open mouths of the volunteers. Then they coughed in the volunteers’ faces five times. “I may say that the volunteers were perfectly splendid about carrying out the technic of these experiments,” Rosenau noted. “They were inspired with the thought that they might help others.” The researchers also sprayed a filtered solution made from 13 strains of Pfeiffer’s bacillus into the volunteers’ throats and eyes, and later injected the volunteers with blood from flu patients.
No one got sick.
Rosenau didn’t draw any conclusions, though, and only underscored the mystery they faced: “We entered the outbreak with a notion that we knew the cause of the disease. Perhaps, if we have learned anything, it is that we are not quite sure what we know.”
Finding the real flu virus
Some teams insisted that Pfeiffer’s bacillus vaccines were effective—physicians in New Orleans, for example, claimed theirs prevented 90 percent of flu infections. For others, the bacterium had fallen further out of favor. By the time a third wave of the pandemic hit in early 1919, vaccines containing a mixture of dead bacteria were more common than ones purely focused on Pfeiffer’s bacillus. These treatments didn’t help with the flu, but they seem to have reduced overall fatalities by preventing bacterial pneumonia, a common secondary infection during the pandemic.
For a worried public, confusion reigned about what really caused the flu.

In March 1919 the Kansas City Kansan spoke to Noble P. Sherwood, head of the University of Kansas’s bacteriology department, about reports that his team had identified the actual flu germ. He denied it. “The ‘flu’,” the newspaper snarked, “has the scientific world up in a tree, out on a limb, in deep water, gagged, bound hand and foot, yet waving both hands and waving wildly for help.” (Find out what lessons we can learn from the history of 1918 flu fatigue.)
Flu deaths finally returned to pre-pandemic levels in 1921, and for the next nine years scientists tried—and failed—to definitively rule out Pfeiffer’s bacillus as the causative agent, in part because seasonal flu continued to ravage communities who had no effective treatments. Even a 500-page global review of all pandemic-related scientific papers could only conclude that “it cannot be legitimately deduced that the Pfeiffer bacillus … either is the cause or not the cause of influenza,” as bacteriologist Edwin Jordan wrote in 1927.
Things finally turned around in 1930, when virologist Richard Shope isolated the first known flu virus in sick pigs in Iowa. Inspired by Shope, scientists in the U.K. swabbed the throats of flu-stricken people and injected a filtered fluid into ferrets. The animals promptly fell ill. The team also swabbed Pfeiffer’s bacillus into the animals’ noses, and it had no effect.
“We consider that the evidence given above strongly suggests that there is a virus element in epidemic influenza,” the English researchers wrote in 1933.
They were right. It had taken roughly 40 years, thousands of studies, and tens of millions of deaths, but scientists had finally found the real cause of pandemic influenza. A full 72 years later, in 2005, Taubenberger and his colleagues were able to pinpoint the deadly strain that caused the 1918 pandemic using tissues from a woman preserved in Alaskan permafrost. It was H1N1, and it had leapt from birds to humans.
H1N1 is the ancestor of some seasonal flu viruses that have infected us since, says Taubenberger, and it gets the blame for many flu-related fevers, shivers, coughs, and lost days of work.
“So in a sense, we’re still in the 1918 flu era more than a hundred years later. That’s a really profound thing for me,” he says. “At least 50 million people died in the pandemic in 1918, but tens of millions of people have died in the past century because of seasonal flu and subsequent pandemics—all because of this single introduction of a virus a hundred years ago.”

Casting a long shadow
Despite the chaos it caused in 1918—or arguably because of it—Pfeiffer’s bacillus had a lasting effect on medicine and microbiology.
Then as now, researchers trying to control the pandemic were publishing their findings about causes and treatments at a frantic pace. But in 1918 it was much harder to compare results, let alone understand the big picture. The public health community at the time had no standardized methods of research or testing, virtually no peer review, and no common protocols for clinical trials. Some of the vaccine trials for the 1918 flu were conducted on vulnerable populations, including mentally ill patients, orphans, and prisoners.
In response, the American Public Health Association issued the nation’s first guidelines for conducting vaccine trials in January 1919. The guide included some of the most foundational practices used today, such as having a control group—a set of participants who don’t get the experimental treatment and so serve as a baseline—and matching participants in the control and experimental groups by gender, age, and prior exposure.
In 1928 “a very bad year of seasonal influenza got Congress worried,” so they created the National Institutes of Health, says historian John Barry, author of The Great Influenza. “Had 1918 not sensitized them, it wouldn’t have happened.”
Similarly spurred by the missteps of the 1918 pandemic, the World Health Organization established a network of 26 laboratories around the world called the Global Influenza Surveillance and Response System in 1952. Taubenberger says scientists were thus better prepared when the H2N2 pandemic hit in 1957. They were ready with antibiotics to treat the secondary infections that had been so devastating in 1918, and they could quickly create effective vaccines for the specific strain.
Also, one upside of chasing down Pfeiffer’s bacillus—also known as Haemophilus influenzae, or H. flu—was that researchers learned more about it. In 1929 a young bacteriologist named Margaret Pittman studied more than 500 mucus samples from Rockefeller Hospital patients. She was trying to definitively establish or completely sever the link between the bacterium and the flu, and she didn’t do either. But she did discover six encapsulated strains of H. flu. Humans are H. flu’s only host, and some strains live harmlessly in our noses and throats. But one strain, now known as Hib, is especially pathogenic.
Pittman’s work revealed Hib as the cause of a variety of serious conditions, including influenzal meningitis, which can lead to death or lifelong disabilities. Soon after her discovery, Pittman developed a serum from horse blood that saved tens of thousands of children and made her internationally famous. Her insights were instrumental in the creation of the Hib vaccine 50 years later, which has since virtually eradicated Hib diseases wherever it’s been introduced.
An historic coronavirus, too?
Recently scientists have found hints that Pfeiffer’s mistake may not have been the only error associated with the 1889 pandemic. If they’re right, the discovery could have implications for the COVID-19 pandemic.
In a 2005 paper Belgian researcher Leen Vijgen traced the most common ancestor of a bovine coronavirus and the human coronavirus CO43 to around 1890, when it seems to have leapt from cows to people. Other scientists have since argued that the disease seen in 1889 shares similar symptoms to those of COVID-19, including the loss of taste and smell, seizures, and long recovery periods.
Perhaps, they say, the 1889 pandemic was not caused by a flu virus at all, but by the CO43 coronavirus. Teasing out the truth may offer a window into the future of SARS-CoV-2; for one, the strain of CO43 circulating today causes only mild symptoms.
Taubenberger and his NIAID colleague David Morens have also set their sights on the 1889 pandemic. They’re seeking tissue samples from the period, which have so far proven elusive.
“It’s very, very hard to find autopsy samples from before 1918,” Taubenberger says. “We have been working very hard with other collaborators around the world to find such cases, and we’ve been analyzing autopsy cases going back to about 1907 or so. No one is aware of any tissues from the 1890s. But that's not to say they don’t exist somewhere.”
Taubenberger adds that it’s a modern mistake to think the researchers working during past pandemics were missing the obvious: Despite having vastly better technology and improved understanding of how viruses cause disease, we’re still in the dark about some aspects of COVID-19, including its origins, its long-term impacts on the body, and its ultimate evolutionary trajectory. Today’s scientists have also had to navigate conflicting data about how COVID-19 spreads and how best to control it.
“If you don’t know what the unknowns are, you can’t look for them,” Taubenberger says. “We don’t know what our unknowns are. A hundred years from now, there are definitely going to be insights that should have been quote-unquote ‘obvious’ to us now. And that’s perfectly fine. That’s the way of science.”
Go Further
Animals
- How can we protect grizzlies from their biggest threat—trains?How can we protect grizzlies from their biggest threat—trains?
- This ‘saber-toothed’ salmon wasn’t quite what we thoughtThis ‘saber-toothed’ salmon wasn’t quite what we thought
- Why this rhino-zebra friendship makes perfect senseWhy this rhino-zebra friendship makes perfect sense
- When did bioluminescence evolve? It’s older than we thought.When did bioluminescence evolve? It’s older than we thought.
- Soy, skim … spider. Are any of these technically milk?Soy, skim … spider. Are any of these technically milk?
Environment
- Are the Great Lakes the key to solving America’s emissions conundrum?Are the Great Lakes the key to solving America’s emissions conundrum?
- The world’s historic sites face climate change. Can Petra lead the way?The world’s historic sites face climate change. Can Petra lead the way?
- This pristine piece of the Amazon shows nature’s resilienceThis pristine piece of the Amazon shows nature’s resilience
- Listen to 30 years of climate change transformed into haunting musicListen to 30 years of climate change transformed into haunting music
History & Culture
- Meet the original members of the tortured poets departmentMeet the original members of the tortured poets department
- Séances at the White House? Why these first ladies turned to the occultSéances at the White House? Why these first ladies turned to the occult
- Gambling is everywhere now. When is that a problem?Gambling is everywhere now. When is that a problem?
- Beauty is pain—at least it was in 17th-century SpainBeauty is pain—at least it was in 17th-century Spain
Science
- Here's how astronomers found one of the rarest phenomenons in spaceHere's how astronomers found one of the rarest phenomenons in space
- Not an extrovert or introvert? There’s a word for that.Not an extrovert or introvert? There’s a word for that.
- NASA has a plan to clean up space junk—but is going green enough?NASA has a plan to clean up space junk—but is going green enough?
- Soy, skim … spider. Are any of these technically milk?Soy, skim … spider. Are any of these technically milk?
Travel
- Could Mexico's Chepe Express be the ultimate slow rail adventure?Could Mexico's Chepe Express be the ultimate slow rail adventure?
- What it's like to hike the Camino del Mayab in MexicoWhat it's like to hike the Camino del Mayab in Mexico







