Recommended
In the response to the COVID-19 pandemic, it is now evident that many of the public health and hospital-based interventions deployed by high-income countries (HICs) may be ineffective or infeasible in low- and middle-income countries (LMICs). Social distancing including lockdowns, rapid deployment of effective test-and-trace protocols followed by quarantine, the ability to properly self-isolate, effective protection of hospital staff from infection with appropriate PPE, and upscaled hospital care – many of these interventions cannot be implemented in the time frame required, or carry consequences so significant that they are socio-politically unacceptable. In this piece, we sound caution about the feasibility of lockdowns and isolation in LMICs, and the cost-effectiveness of putting large-scale resources into upscaled hospital care. We also suggest a different order of priority for immediate next steps.
While WHO and Africa CDC have published guidance, policymakers are asking tough questions and we have few answers at this time:
- In many LMICs, the health system, particularly hospitals, was already overwhelmed by demand prior to the pandemic. The clinical guidelines suggest upscaled hospital care including nasal oxygen, mechanical ventilation and, for those that survive ventilation but have complications, dialysis. But resources are extremely limited. In India, for example, the Center for Disease Dynamics, Economics, and Policy estimates that there are 30-50,000 ventilators available when 1 million will be required at the peak of the COVID-19 outbreak, and there are only 1,850 nephrologists available to supervise dialysis in a country where an estimated 3% of deaths in the 15-64 year old population are from renal failure each year at baseline. In this context, can countries realistically raise hospital capacity quickly? And if not, would “flattening the curve” by social distancing make any real difference to the (in)ability of the health system to respond now or in the future? Even with best practice and infrastructure, ICU response outcomes in high-incomes have been dismal (possibly an artifact of the way high-income health systems like Italy are classifying deaths with COVID rather than from COVID)–but at face value, these outcomes beg the question of whether more ICU is the best investment?
- If more than 60 percent of the workforce is in the informal sector and must work no matter what to survive, can “stay-at-home” orders result in fewer cases, or does “stay-at-home” lead to more detentions, transmission, social disorder, and impoverishment, including more deaths from non-COVID-19 related illness?
- Can people who live in the most densely occupied households and neighborhoods in the world isolate their vulnerable and elderly? In India, for example, about 73 percent of households reported living in two rooms or less in the last census.
- In the few models that consider LICs, recommended interventions such as test-trace-isolate and/or social distancing measures, even when assuming a modest basic reproduction number for the virus, must reach effectiveness levels comparable or above those achieved in certain high income settings (such as South Korea and Singapore) in order to significantly flatten the curve. Is this even remotely realistic?
Despite these important questions, a large share of the new World Bank health sector operations and restructuring seems to be focused on hospital-oriented care–sourcing and sending PPE, tests, and especially ventilators as is the WHO Strategic Preparedness and Response Plan. USAID recently circulated a draft request for quotes to buy 100,000 ventilators through the Global Health Supply Chain project as another example. While more analysis is needed, given the current spread and the likely trajectory of the outbreak in LMICs, should money go towards a different set of priorities?
We have three suggestions to focus on the broader protection of life in the immediate term that are different in scale from existing guidance:
- Start with water and sanitation: Immediately scale up low-tech clean water and handwashing interventions and more toilet facilities (which will do good beyond the COVID-19 pandemic and save lives from non-COVID-19 infectious diseases as well).
- Protect other essential healthcare services and supply chains like vaccination, malaria control, insulin, antihypertensives, and reproductive, maternal, and child health, where most lives may be lost. Baird et al (REStat 2011) estimated that a 1 percent decrease in per capita GDP in developing countries was associated with a 0.24 to 0.40 increase in infant mortality per 1,000 children born. For developing countries in East Asia and the Pacific, the World Bank has already projected a decline in GDP growth of 3.7 percentage points in 2020. Extrapolating these figures, a back-of-the-envelope calculation from our colleague Justin Sandefur suggests that if a similar economic downturn occurs in other regions, it would imply between 100,000 to 200,000 additional infant deaths in developing countries worldwide next year–even without any epidemic deaths in the developing world. This must be avoided at all costs.
- Cash transfers to stay home: The enormous economic consequences of COVID-19 are sufficient motivation for a scale-up of cash transfers in LMICs. But if social distancing is our only hope to slow spread, perhaps most of the money should go directly to households to enable “stay-at-home” and not spent on ventilators and dialysis equipment that cannot be effectively utilized in the near-or medium-term.
We also recommend some changes consistent with existing guidance but that require a different kind of prioritization in LMIC settings:
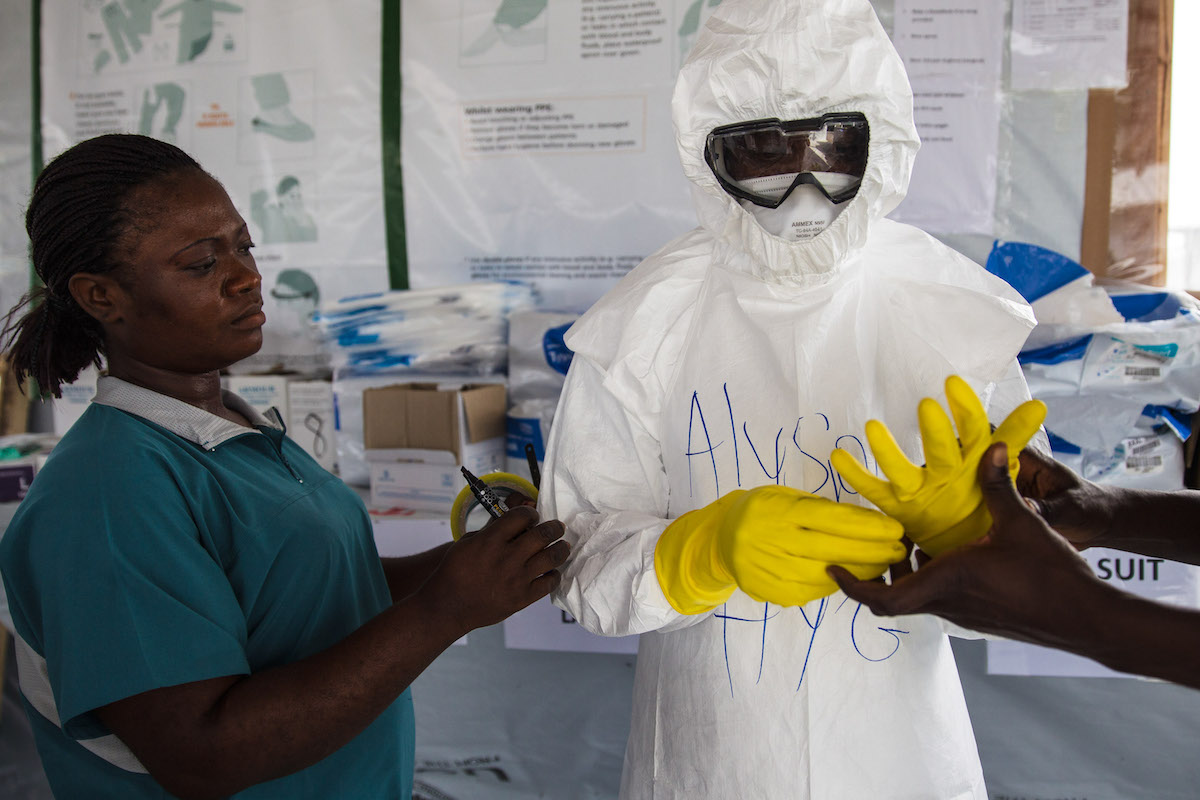
- Protect the health workforce: Prioritize testing and PPE (basic and N95 masks for invasive ENT procedures) for frontline healthcare staff, as large chunks of the limited to start with human resource capacity can quickly fall sick.
- Target tests: Provide testing to key public hospitals and community settings where patients are likely to show up in order to rapidly determine their COVID-19 status; in parallel, conduct random population testing to determine the virus’ prevalence.
- Use real world national and subnational data to inform modelling forecasts: Set up a central facility (coordinated perhaps by the African CDC or other regional bodies) to collect and analyze data on COVID-19 hospitalizations, critical care (where available), deaths and discharges, by age subgroup and comorbidities. This is crucial for evidenced-based policy, including estimation of impact of alternative interventions (as opposed to importing Chinese or EU estimates), and should be shared regularly with crisis response leads.
- Develop triage protocols for ventilation: For those settings able to harness both trained personnel and equipment for invasive mechanical ventilation, develop rigorous triage mechanisms. There are curated pieces on critical care triage in high-income settings (also here for what UK is doing in real time), but there is limited available from LMIC health professionals and systems. Locally developed guidelines would be most ideal.
There is a need for more tailored guidance in LMICs, and perhaps a different emphasis in spending (e.g. away from the tertiary care, high-tech focus currently challenged by some even in the European context) than has thus far been the case as informed by high-income countries. There are no easy answers, but we must attempt to answer some of the pressing questions now as LMICs across the world prepare for the COVID-19 wave that has swamped Europe and North America. Your feedback is welcome.
Thanks to Justin Sandefur for comments and calculations.
Correction: We initially misstated the number of deaths from renal failure each year in India. 3% of yearly deaths for the 15-64 population are from renal failure, not that 3% of that population dies each year from renal failure.
Disclaimer
CGD blog posts reflect the views of the authors, drawing on prior research and experience in their areas of expertise. CGD is a nonpartisan, independent organization and does not take institutional positions.
Image credit for social media/web: everythingpossible via Adobe Stock