It’s a science lesson you probably learned in grade school: You can only catch certain illnesses, like the flu, from another person. But a new paper argues that many diseases seen as noncommunicable, like most cancers and heart disease, might be transmissible sometimes—thanks to the seemingly harmless microbes living in and on our bodies.
Every one of us is a walking zoo, filled to the brim and positively coated with bacteria, viruses, and other assorted invisible creatures that depend on our bodies for sustenance and a place to have sex on. Terrifying as this reality might seem, these critters typically co-exist with us without causing any harm, and many are beneficial, such as the bacteria in our gut that break down foods.
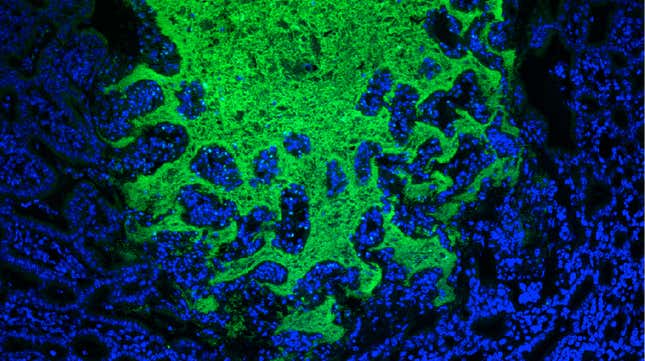
Scientists have coined the unseen world where these microbes live the microbiome. In recent years, we’ve begun to unravel the complex ways the microbiome can affect our bodies, especially when it’s thrown out of balance. Studies involving lab animals and humans, for instance, have linked a variety of chronic, noncommunicable conditions like obesity and cardiovascular disease to an out-of-whack microbiome (scientists call it dybiotic instead).
We’re still in the early stages of understanding the microbiome. But in a new paper published Thursday in the journal Science, the authors argue that there’s enough evidence to start testing out the theory that many noncommunicable diseases can be transmissible via the microbiome.
For one, conditions like obesity is known to cluster in groups of people. A large study of more than 12,000 people across a 30-year span of time, for instance, found that people who had an obese friend were 57 percent more likely to be obese themselves; a similar pattern existed for those who had an obese spouse or a sibling who became obese in their adulthood.
In animals, studies have shown that if you wipe out the gut microbiome of healthy mice and transplant a microbiome sourced from obese mice, the former group of mice are more likely to become obese than control mice. Studies of the reverse concept—altering the microbiomes of sick mice to make them resemble healthy mice—have also been shown to treat or slow the progression of not only obesity but other chronic ailments, like Alzheimer’s and heart disease.
There’s even some early evidence of human-to-human transmission of our microbiomes in general, such as from mother to child in the womb or from other people’s fecal bacteria that ends up in our food and water.
“When you add up these [data], it makes a compelling case,” lead author Brett Finlay, a microbiologist at the University of British Columbia in Canada, told Gizmodo via email.
Their theory is more complicated than the germ theory that explains why the flu virus spreads from person to person every winter, though.
Obesity can run in groups, but a shared environment or genetics undoubtedly accounts for some of that increased risk. At the same time, environment and genetics also shape what our microbiomes look like. And even if there is such a thing as a “risky” microbiome for Alzheimer’s, it’s not as if someone with that microbiome will wake up with dementia the next morning. Many chronic conditions take years, if not decades, to emerge even in people at high risk of them, and not everyone with that risk will become sick. Finlay also noted that we’re not talking about a single bad germ, but a microbiome that may have gone off-kilter in any number of ways.
All these challenges make the theory hard to prove. But the authors say they’ve developed rules to guide ongoing and future research, based on the criteria established by Robert Koch and others in the late 18th century to prove a specific germ was causing a specific disease (otherwise known as Koch’s postulates).
They include showing that certain patterns of microbes are more commonly found in people with a non-communicable disease but not healthy populations; being able to grow these microbes in the lab; showing that healthy lab animals can develop the same disease when the microbes are transplanted over; and lastly being able to find a similar pattern of microbes in the now-sick animals.
“The general concepts of microbe transmission apply,” Finlay said. “The hardest part of the theory is uncoupling environment and diet from microbes, as they go hand in hand.”
Plenty of scientists are already studying the links between human disease and the microbiome. We’re even on the verge of routinely using poop transplants to treat certain ailments. But it’s going to take a long time and lots of research before we could start thinking of noncommunicable diseases as sometimes contagious, much less be able to reliably treat them through the microbiome. And we’ve only really studied bacteria in the microbiome, mostly in the gut; there are untold numbers of viruses and fungi living inside us too.
But by publishing about their theory now, Finlay and his co-authors hope to spark more interest from their fellow scientists.
“They are compelling arguments, and this could have a large effect on health policy issues,” he said. “However, nobody has proposed the concept before, and it warrants a closer look.”
This article has been updated with comments from the paper’s lead author.