Abstract
Purpose
Function describes an individual’s ability to perform everyday activities. In the context of cardiac surgery, functional changes quantify the effect of surgery on one’s day-to-day life. Decreases in regional cerebral oxygen saturation (rScO2) measured using near-infrared spectroscopy (NIRS) has been associated with postoperative cognitive decline but its relationship with function has not been studied. We sought to determine the feasibility of conducting a large observational study examining the relationship between decreases in rScO2 during cardiac surgery and postoperative functional decline.
Methods
We undertook a single-centre, pilot sub-study of the NeuroVISION-Cardiac Surgery pilot study, which included adults undergoing isolated coronary artery bypass grafting on cardiopulmonary bypass; all patients enrolled in NeuroVISION-Cardiac Surgery were included. Function was evaluated at baseline, 30 days, and three months using the Standardized Assessment of Global activities in the Elderly (SAGE) scale. Blinded NIRS monitors were affixed for the duration of surgery. Our feasibility outcomes were to recruit one patient per week, obtain complete NIRS data in ≥ 90%, obtain SAGE at all time-points in ≥ 90%, and determine the time required for NIRS data to be transcribed into case report forms.
Results
49/50 patients enrolled in NeuroVISION-Cardiac Surgery were recruited over 48 weeks (1.02 patients/week). Of the 49 included patients, 49 (100%) had complete NIRS data and 44 (90%) had complete SAGE data. The time required for NIRS data collection was a mean (standard deviation) of 5.5 (1.8) min per patient.
Conclusion
This pilot study shows the feasibility of conducting a large observational study examining the relationship between decreases in cerebral saturation during cardiac surgery and postoperative functional decline.
Trial registration
www.clinicaltrials.gov(NCT04241289); registered 27 January 2020.
Résumé
Objectif
La capacité fonctionnelle constitue la capacité d’une personne à accomplir des activités quotidiennes. Dans le contexte d’une chirurgie cardiaque, les changements fonctionnels permettent de quantifier l’effet de la chirurgie sur le quotidien des individus. Les baisses de la saturation en oxygène cérébral régional (rScO2) mesurées à l’aide de la spectroscopie proche infrarouge (NIRS) ont été associées à un déclin cognitif postopératoire, mais leur relation par rapport à la capacité fonctionnelle n’a pas été étudiée. Nous avons tenté de déterminer s’il était possible de réaliser une vaste étude observationnelle examinant la relation entre les baisses de rScO2 pendant une chirurgie cardiaque et le déclin fonctionnel postopératoire.
Méthode
Nous avons entrepris une sous-étude pilote monocentrique de l’étude pilote NeuroVISION-Cardiac Surgery, qui incluait des adultes subissant une chirurgie de pontage aortocoronarien sous circulation extracorporelle; tous les patients recrutés dans l’étude NeuroVISION-Cardiac Surgery ont été inclus dans ce volet. La capacité fonctionnelle a été évaluée avant l’opération, puis à 30 jours et trois mois à l’aide de l’échelle SAGE (Standardized Assessment of Global activities in the Elderly, soit Évaluation standardisée de la fonction globale chez la personne âgée). Des moniteurs de NIRS étaient installés pour toute la durée de la chirurgie sans que les valeurs ne soient connues de l’équipe traitante. Nos critères de faisabilité consistaient à recruter un patient par semaine, obtenir des données de NIRS complètes pour ≥ 90 % des patients, obtenir des données de SAGE pour tous les points dans le temps pour ≥ 90 % des patients, et déterminer le temps nécessaire à retranscrire les données de NIRS dans les formulaires d’étude de cas.
Résultats
Au total, 49/50 patients recrutés dans l’étude NeuroVISION-Cardiac Surgery ont été recrutés sur une période de 48 semaines (1,02 patients/semaine). Parmi les 49 patients inclus, les données de NIRS ont été obtenues pour 49 (100 %) patients et les données de SAGE pour 44 (90 %) patients. Le temps nécessaire à la collecte de données de NIRS était en moyenne (écart type) de 5,5 (1,8) min par patient.
Conclusion
L’étude pilote a démontré la faisabilité d’une vaste étude observationnelle examinant la relation entre les baisses de la saturation cérébrale pendant la chirurgie cardiaque et le déclin fonctionnel postopératoire.
Enregistrement de l’étude
www.clinicaltrials.gov(NCT04241289); enregistrée le 27 janvier 2020.
Similar content being viewed by others
More than 1 million patients around the world undergo cardiac surgery annually.1,2 With longevity comes comorbidity and, in the context of an aging population, the number of people requiring cardiac surgical procedures is rising.1,2 Improvements in intraoperative management and perioperative care have substantially reduced perioperative morbidity and mortality.3 Nevertheless, postoperative cognitive impairment remains common and constitutes one of the most devastating and feared sequelae of cardiac surgery, particularly among the elderly population. Although cognitive decline is a patient-important outcome, the way it is currently measured—using psychometric tests—has limited meaning for non-experts. In addition, the relationship between change in cognitive test scores and daily function remains unknown.
Function is a multi-dimensional construct that describes an individual’s ability to perform everyday activities and can be broken down into the following: 1) activities of daily living (ADL) (i.e., daily self-care activities, including bathing, dressing, and eating), 2) instrumental activities of daily living (IADL) (i.e., activities that are not necessary for basic function, but allow an individual to live independently in the community, including housework, managing finances, and shopping), and 3) applied cognition, upon which the other two functional dimensions are predicated. Functional ability is an indicator of overall health. In the context of surgical procedures, functional changes quantify the implications of having had a procedure on one’s day-to-day life. Unfortunately, little is known about mitigating functional decline after cardiac surgery, and no modifiable risk factors have been identified.
Near-infrared spectroscopy (NIRS) is a non-invasive technique that can be used to continuously monitor regional cerebral oxygen saturation (rScO2), which represents the balance between cerebral oxygen delivery and consumption.4 In adult patients undergoing cardiac surgery, regional cerebral oxygen desaturation measured using NIRS has been associated with postoperative cognitive decline (POCD),5 although it has not been studied in relation to functional decline.
It has been shown that anesthesiologists are able to reverse cerebral desaturations.6 If a relationship between cerebral desaturation and functional decline was established, it might represent a modifiable risk factor that could be targeted for intervention. Nevertheless, before this trial can be undertaken, a large observational study examining the relationship between decreases in intraoperative rScO2 and postoperative functional decline needs to be conducted. This study would also need to establish the optimal prognostically important rScO2 threshold associated with patient-important outcomes. The thresholds evaluated in the literature vary widely and are limited by small sample sizes.5 It is unclear whether the optimal rScO2 target should be an absolute rScO2 value, a proportional decrease from baseline rScO2 value, or the duration of time below a given rScO2 value. To assess the feasibility of conducting a large observational study to determine the optimal prognostically important rScO2 threshold associated with postoperative cognitive and functional decline, we performed a pilot sub-study of NeuroVISION-Cardiac Surgery.
Methods
Study design
ReFUNCTION was a prospective, observational pilot sub-study of the NeuroVISION-Cardiac Surgery pilot study, whose objective was to establish the feasibility of conducting a large study to evaluate the incidence of covert stroke in adult patients undergoing coronary artery bypass grafting (CABG) and to evaluate the relationship between covert stroke and postoperative delirium and POCD.
Patients
All participants in NeuroVISION-Cardiac Surgery were included in the ReFUNCTION pilot study. Patients were included in NeuroVISION-Cardiac Surgery if they were ≥ 21 yr old, scheduled to undergo isolated CABG on cardiopulmonary bypass using a median sternotomy approach at the Hamilton General Hospital, Hamilton, Ontario, Canada, and had at least one of the following preoperative risk factors: cerebrovascular disease, peripheral vascular disease, renal insufficiency (estimated glomerular filtration rate < 60 mL·min−1·1.73 m−2), diabetes mellitus (on an oral hypoglycemic agent or insulin), urgent surgery (i.e., inpatient awaiting revascularization for acute coronary syndrome or myocardial infarction), recent (within the past year) smoker, or left ventricular ejection fraction < 35%. Patients undergoing emergency or repeat surgery, in whom intraoperative circulatory arrest was planned, who were previously diagnosed with dementia, or who had a contra-indication to magnetic resonance imaging (MRI) were excluded.
Recruitment
Research staff screened potential participants in surgical clinics, preoperative assessment clinics (PAC), cardiac surgery wards, and cardiac care units (CCUs). They used a variety of approaches (e.g., screening the daily surgical list, review of patients in the preoperative holding area, cardiac surgical wards or CCUs) to capture patients admitted through the emergency department and who did not attend the PAC. All NeuroVISION-Cardiac Surgery study patients were concurrently asked to provide informed consent for ReFUNCTION.
Outcomes
The ReFUNCTION pilot feasibility outcomes were as follows: 1) to recruit on average one patient per week, 2) to obtain in ≥ 90% of patients complete intraoperative NIRS data (i.e., a recording transcript that was within 15% of the duration of the surgical procedure), 3) to collect complete functional (Standardized Assessment of Global activities in the Elderly [SAGE] scale) outcome data at baseline, 30 days, and three months in ≥ 90% of patients, and 4) to collect data on the time required for the study research assistant to download and transcribe intraoperative data. These four objectives were selected both to ensure feasibility and to inform planning for the main trial. We chose to assess recruitment rate because, if a large study of NIRS is conducted in conjunction with a study using MRI, recruitment will be limited by the availability of MRI and the fact that many postoperative cardiac surgery patients are unable to undergo MRI because of permanent or temporary epicardial pacemakers. We sought to assess the completeness of recording transcripts because few studies report the completeness of intraoperative NIRS data obtained and, if practitioners are blinded to NIRS values, a NIRS strap that loses contact with the patient or becomes disconnected from the monitor is unlikely to be corrected. We chose to assess the completeness of functional outcome follow-up as studies examining cognitive outcomes often have high and non-random loss to follow-up; it is unknown whether functional outcomes are similarly affected. Finally, we sought to assess NIRS data collection time as this is an important process outcome for planning a large trial.
The SAGE is a 15-item, composite measure of physical and cognitive functioning that was developed to measure functional decline in patients with vascular disease. It measures all three functional domains (ADL, IADL, and cognition), is cross-culturally generalizable, and can be completed by a patient or their caregiver in person or over the phone within 15 min. Each item within the scale relates to one of the three functional domains, and can be evaluated alone, in combination with other items from the same functional domain, or as a composite measure of global function. Higher SAGE scores denote greater functional impairment. SAGE has previously been validated in the cerebrovascular disease population although this data has not been published. Our group has also validated SAGE in the cardiac surgery population within a sub-study of VISION-Cardiac Surgery7; the manuscript is in submission.
Study procedures
Table 1 provides an overview of the procedures involved in both the NeuroVISION-Cardiac Surgery and the ReFUNCTION pilot studies. The Montreal Cognitive Assessment (MoCA) and Digit Symbol Substitution (DSS) test were performed preoperatively, at hospital discharge, and at the initial follow-up visit four to six weeks after surgery. The SAGE was performed preoperatively, at the initial follow-up visit, four to six weeks after surgery, and by telephone follow-up at three months after surgery. Delirium was assessed daily until discharge using the Confusion Assessment Method-Intensive Care Unit (CAM-ICU)8,9 while patients were in the ICU and using the 3D-Confusion Assessment Method (3D-CAM)10 while patients were on the cardiac surgery ward. The research assistants who were responsible for cognitive and functional outcomes assessment were blinded to whether the patient had an intraoperative decrease in rScO2 or whether postoperative covert stroke was detected on MRI.
Bilateral NIRS monitoring straps were affixed to patients’ foreheads by a trained research assistant in the operating room before the start of anesthesia. The monitoring straps were connected to an InVOS 5100C (Medtronic, USA) NIRS monitor, whose screen was securely covered for the purposes of blinding. Baseline rScO2 was recorded before the start of anesthesia. Monitors were removed at the end of the cardiac surgical procedure before patients left the operating room.
Participants underwent a single MRI scan of the head with T1, T2 Flair, and diffusion-weighted sequences between postoperative day 3 and 9. Scans were read at a core lab by a trained radiologist blinded to the clinical status of the patient.
Statistical analysis
No formal sample size was calculated; we sought to study a convenience sample of 50 patients, which was the size of the NeuroVISION-Cardiac Surgery sub-study. Based on our stated objectives, we believed that 50 patients would be adequate to obtain the feasibility information required.
As this was a pilot study designed to assess feasibility, we did not undertake hypothesis testing. Binary and categorical variables are reported as counts and proportions and continuous variables are reported as mean (standard deviation [SD]) or median [interquartile range (IQR)] as appropriate. We report results as the difference between estimates with a 95% confidence interval (CI). Baseline demographics and cognitive and functional test scores are presented according to two thresholds that have been previously identified as clinically important: 1) a ≥ 20% decrease in intraoperative rScO2 from recorded baseline6 and 2) any rScO2 less than an absolute value of 50.11 We defined POCD as a postoperative MoCA score that was ≤ 2 points below the baseline MoCA score. We defined functional decline as the development of new “mild” impairment in any two SAGE functional parameters or the development of new “moderate” or “severe” impairment in a single SAGE functional parameter.
Results
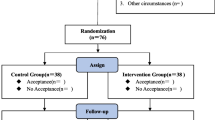
The Figure provides an overview of the ReFUNCTION study flow. A total of 66 participants were enrolled from March 2017 to February 2018; of these, 50 (76%) ultimately underwent an MRI scan and were included in NeuroVISION-Cardiac Surgery. One patient did not have complete intraoperative NIRS monitoring data because the research assistant was not present to apply the blinded NIRS monitor, resulting in 49/50 participants (98%) being included in ReFUNCTION.
Table 2 presents baseline demographics, neurocognitive test scores, and functional test scores according to the presence of ≥ 20% decline from baseline rScO2 during surgery and the presence of any rScO2 value below 50. We present data in this manner for interest only; our study was not powered to allow for comparisons between groups. The mean (SD) age of all patients was 66 (9) yr, 14% were female, and their mean (SD) Euroscore12 was 4.8 (2.4). The mean (SD) MoCA and DSS scores at baseline were 24.1 (3.1) and 43.5 (14.0), respectively. The median [IQR] SAGE score at baseline was 2 [0–3]. Patients who experienced an intraoperative decrease in rScO2 using either definition were more likely to be female, representing 26% of those who had intraoperative cerebral desaturation and 4% of those who did not have intraoperative cerebral desaturation. There was no difference in baseline cognitive and functional test scores between patients who had intraoperative cerebral desaturation and patients who did not have intraoperative cerebral desaturation, regardless of which definition was applied.
Table 3 describes the feasibility outcomes of the ReFUNCTION pilot study. Forty-nine patients were recruited over 48 weeks, with an average recruitment rate of 1.02 patients per week. Of the 49 patients who were included in the study, 49 (100%) had a complete intraoperative NIRS transcript (i.e., a recording within 15% of the time in minutes between when the patient entered the operating room before surgery and left the operating room after surgery). Among all patients, 48/49 (98%) had a baseline SAGE scale (insufficient time before surgery to complete), 47/49 (96%) had a 30-day SAGE scale (one patient’s medical condition did not allow for assessment, one patient refused to follow-up), and 46/49 (94%) had a three-month SAGE scale (one death, two refusals to follow-up). 44/49 (90%) of patients had a SAGE scale at each of these three time-points. There was no difference in SAGE completion rates between the patients who had intraoperative rScO2 decline and those who did not have intraoperative decline using either definition. The mean (SD) time in minutes required for the research assistant to transcribe the intraoperative NIRS transcript into the study case report forms (CRFs) was 5.5 (1.8) min.
Table 4 describes patients’ neurocognitive and functional outcomes according to the two pre-established NIRS desaturation thresholds. We present data in this manner for interest only; our study was not powered to allow for comparisons between groups. There were no differences between groups (using either definition of rScO2 desaturation) in postoperative delirium, new lesions detected on MRI, neurocognitive test scores at discharge and 30 days, SAGE score at 30 days and three months, and POCD. Among all patients, the mean (SD) MoCA scores at discharge and 30 days were 24.9 (3.6) and 26.2 (3.1) and the mean (SD) DSS at discharge and 30 days were 46.4 (16.3) and 57.3 (15.4). The median [IQR] SAGE score was 0 [0–2] at 30 days and 0 [0–1] at three months. Overall, 9 (21%) patients had POCD at discharge and 3 (7.9%) patients had POCD at 30 days. The overall incidence of functional decline was 26% at 30 days and 26% at three months. There was no difference in the incidence of functional decline between patients who did or did not have a decrease in rScO2 that was greater or equal to 20% of their baseline value. Patients who had any rScO2 value below 50 were more likely to have functional decline at 30 days when compared with those in whom all values were 50 or greater, with an incidence of 39% (9/22) compared with 12% (3/25). This difference was no longer present at three months.
Discussion
The ReFUNCTION pilot study shows the feasibility of conducting a large, observational study to establish the relationship between intraoperative decreases in cerebral oxygen saturation and postoperative function. We were able to recruit a minimum of one patient per week, which satisfies our pre-established feasibility threshold. The ReFUNCTION pilot was a sub-study of NeuroVISION-Cardiac Surgery pilot. For this reason, recruitment was limited by local MRI scan capacity, which is restricted to one scan for research purposes per week. If, in planning for the main trial, it becomes apparent that this recruitment rate is not acceptable, we may consider conducting ReFUNCTION as an independent study. Nevertheless, given the similar objectives of ReFUNCTION and NeuroVISION-Cardiac Surgery, in addition to the improved efficiency and decreased costs from pairing research questions, we believe that addressing these two research questions within the same study is the optimal approach.
We were able to obtain complete intraoperative NIRS transcripts in 100% of patients, which shows the feasibility of collecting complete data pertaining to our exposure variable of interest. The mean time required to download and enter transcript data into the study CRFs was 5.5 min, which shows that there will be minimal research assistant time required to complete this aspect of the study.
Finally, we were able to obtain complete SAGE scale data in 90% of patients, including measurements at baseline, 30 days, and three months after cardiac surgery. Complete collection of SAGE scales is of key importance, as SAGE score represents the primary outcome of our main trial. Previous research has found that patients with lower cognitive status are more likely to be lost to follow-up, resulting in potential attrition bias.13,14 We believe the following features of the SAGE scale will help to minimize potential attrition bias in the full trial: it can be administered in person or over the phone, it does not require specialty training to administer, it is available in more than 15 languages, and it can be completed by patients or their surrogates in under 15 min. The results of our pilot study support this belief.
Postoperative cognitive impairment—as defined by decreases in cognitive test scores—is a recognized entity, affecting 3–79% of patients after cardiac surgery.15 Nevertheless, how these decreases in cognitive test scores affect patient’s functional ability (i.e., applied cognition) may be more important to patients. Functional decline may affect 16–36%16,17 of patients after cardiac surgery, although its true incidence is unclear. Published evidence pertaining to function after cardiac surgery has been limited by small sample sizes, varying definitions of functional decline, and differences in the duration between cardiac surgery and functional assessment. The largest prospective study evaluating postoperative function of cardiac surgery patients measured the Katz ADL index three months after surgery in a cohort of 475 patients ≥ 65 yr of age.16 They found that 16% of all patients and 20% of those ≥70 yr suffered functional decline. This study was used to validate a predictive measure of postoperative decline but did not examine any other predictors. In a study of 190 patients undergoing cardiac surgery, Rudolph et al. found that postoperative delirium was associated with functional decline at one month but not 12 months postoperatively.17 No studies have systematically evaluated short- and long-term functional change in a large cohort of consecutive cardiac surgery patients, nor have individual patient predictors been identified. Our group is currently determining the true incidence and predictors of functional decline in a large, prospective cohort study of patients undergoing cardiac surgery.7 Once these are established, interventions to mitigate perioperative functional decline need to be evaluated.
A potential intervention to mitigate postoperative functional decline in patients undergoing cardiac surgery is intraoperative management guided by cerebral oximetry. Limited research has linked the prevention of intraoperative cerebral desaturation—as measured using cerebral oximetry—to benefits in other patient-important perioperative outcomes.5 A recent meta-analysis of 15 randomized-controlled trials that included 2,057 patients found that anesthesia guided by intraoperative cerebral oximetry was associated with a reduction in the incidence of POCD (relative risk, 0.54; 95% CI, 0.33 to 0.90; P = 0.02; I2 = 85%) compared with standard care.5 Additional outcomes including postoperative delirium, perioperative myocardial infarction, and surgical site infection were examined but did not have a statistically significant relationship with management guided by cerebral oximetry. The authors of this meta-analysis expressed a belief that all results were underpowered, and advocated for a large study evaluating the impact of intraoperative management guided by cerebral oximetry on patient-important outcomes.5 We agree with the authors and believe that one of the primary outcomes of such a large trial should be postoperative functional decline.
Before conducting a randomized-controlled trial, a large observational study is required to (i) firmly establish the relationship between intraoperative decreases in rScO2 and (ii) determine the optimal rScO2 value that has a prognostically important relationship with postoperative patient-important outcomes, including functional decline.18 In the ReFUNCTION pilot, we have established the feasibility of conducting this large observational study. To identify the optimal rScO2 value, we will build a logistic regression model to confirm the relationship between intraoperative rScO2 and postoperative functional decline. In doing so, we will control for other important determinants of rScO2 and functional decline, including patient and surgical characteristics, time on cardiopulmonary bypass, pump flow, hematocrit, and O2 saturation. We will use the Mazumdar approach19—a statistical technique previously used to establish the prognostically important cut-point of a continuous variable20—to identify the NIRS value (or change in values) associated with the lowest incidence of postoperative functional decline. The threshold identified will constitute the rScO2 target used in the intervention arm of the full trial. To include 45 covariates in our model and to allow for 20 outcomes per covariate, we will require 900 patients who experience postoperative functional decline. Based on the 25% incidence of three-month postoperative functional decline observed in ReFUNCTION, and assuming a 10% loss to follow-up, we will require a sample size of approximately 4,000 patients undergoing cardiac surgery.
Our pilot study has several strengths. To our knowledge, it is the only study that has evaluated the relationship of intraoperative decreases in rScO2 with postoperative functional ability. Even though the work described here is focused on establishing feasibility, it provides the foundation for future work examining this poorly understood but highly patient-important outcome. We were able to obtain blinded intraoperative NIRS transcripts in all patients and blinded outcomes data including postoperative MRI, cognitive testing, and functional assessment using SAGE. Our pilot study has several limitations, including a small sample size drawn from a single centre. Nevertheless, given that this primary objective of this pilot study was to establish the feasibility of the main study protocol, we believe that the information that we have obtained is adequate to meet our objectives.
Conclusions
Postoperative functional ability is a poorly understood but patient-important outcome. In this pilot study, we established the feasibility of conducting a large observational trial examining the relationship between intraoperative decreases in cerebral oxygen saturation with postoperative functional decline, with the objective to identify a prognostically important threshold for intervention.
References
Wolman RL, Nussmeier NA, Aggarwal A, et al. Cerebral injury after cardiac surgery: identification of a group at extraordinary risk. Multicenter Study of Perioperative Ischemia Research Group (McSPI) and the Ischemia Research Education Foundation (IREF) Investigators. Stroke 1999; 30: 514-22.
Barbut D, Caplan LR. Brain complications of cardiac surgery. Curr Probl Cardiol 1997; 22: 449-80.
Selnes OA, Goldsborough MA, Borowicz LM, McKhann GM. Neurobehavioural sequelae of cardiopulmonary bypass. Lancet 1999; 353: 1601-6.
Zheng F, Sheinberg R, Yee MS, Ono M, Zheng Y, Hogue CW. Cerebral near-infrared spectroscopy monitoring and neurologic outcomes in adult cardiac surgery patients: a systematic review. Anesth Analg 2013; 116: 663-76.
Zorrilla-Vaca A, Healy R, Grant MC, et al. Intraoperative cerebral oximetry-based management for optimizing perioperative outcomes: a meta-analysis of randomized controlled trials. Can J Anesth 2018; 65: 529-42.
Deschamps A, Hall R, Grocott H, et al. Cerebral Oximetry monitoring to maintain normal cerebral oxygen saturation during high-risk cardiac surgery: a randomized controlled feasibility trial. Anesthesiology 2016; 124: 826-36.
Population Health Research Institute. Vascular Events In Surgery patIents cOhort evaluatioN - Cardiac Surgery. Available from: https://clinicaltrials.gov/ct2/show/NCT01842568. NLM identifier: NCT01842568 (accessed May 2020)
Ely EW, Inouye SK, Bernard GR, et al. Delirium in mechanically ventilated patients: validity and reliability of the confusion assessment method for the intensive care unit (CAM-ICU). JAMA 2001; 286: 2703-10.
Ely EW, Margolin R, Francis J, et al. Evaluation of delirium in critically ill patients: validation of the Confusion Assessment Method for the Intensive Care Unit (CAM-ICU). Crit Care Med 2001; 29: 1370-9.
Marcantonio ER, Ngo LH, O’Connor M, et al. 3D-CAM: derivation and validation of a 3-minute diagnostic interview for CAM-defined delirium: a cross-sectional diagnostic test study. Ann Intern Med 2014; 161: 554-61.
de Tournay-Jette E, Dupuis G, Bherer L, Deschamps A, Cartier R, Denault A. The relationship between cerebral oxygen saturation changes and postoperative cognitive dysfunction in elderly patients after coronary artery bypass graft surgery. J Cardiothorac Vasc Anesth 2011; 25: 95-104.
Nashef SA, Roques F, Hammill BG, et al. Validation of European System for Cardiac Operative Risk Evaluation (EuroSCORE) in North American cardiac surgery. Eur J Cardiothorac Surg 2002; 22: 101-5.
Salthouse TA. Selectivity of attrition in longitudinal studies of cognitive functioning. J Gerontol B Psychol Sci Soc Sci 2014; 69: 567-74.
Salthouse TA. Attrition in longitudinal data is primarily selective with respect to level rather than rate of change. J Int Neuropsychol Soc 2019; 25: 618-23.
McGarvey ML, Cheung AT, Stecker MM. Neurologic complications of cardiac surgery. In: Wilterdink JL (Ed.). UpToDate. Available from URL: https://www.uptodate.com/contents/neurologic-complications-of-cardiac-surgery (accessed May 2020).
Hoogerduijn JG, de Rooij SE, Grobbee DE, Schuurmans MJ. Predicting functional decline in older patients undergoing cardiac surgery. Age Ageing 2014; 43: 218-21.
Rudolph JL, Inouye SK, Jones RN, et al. Delirium: an independent predictor of functional decline after cardiac surgery. J Am Geriatr Soc 2010; 58: 643-9.
Nenna A, Barbato R, Greco SM, et al. Near-infrared spectroscopy in adult cardiac surgery: between conflicting results and unexpected uses. J Geriatr Cardiol 2017; 14: 659-61.
Mazumdar M, Smith A, Bacik J. Methods for categorizing a prognostic variable in a multivariable setting. Stat Med 2003; 22: 559-71.
Writing Committee for the VISION Study Investigators, Devereaux PJ, Biccard BM, et al. Association of Postoperative High-Sensitivity Troponin Levels With Myocardial Injury and 30-Day Mortality Among Patients Undergoing Noncardiac Surgery. JAMA 2017; 317: 1642-51.
Author contributions
Jessica Spence contributed to all aspects of this manuscript, including conception and design, acquisition, analysis, and interpretation of data, and drafting the article. Andre Lamy and Jackie Bosch contributed to the conception and design of the study and drafting the article. Lehana Thabane contributed to the analysis and interpretation of data and drafting the article. Stephanie Gagnon contributed to the acquisition, analysis, and interpretation of data and drafting the article. Patricia Power, Austin Browne, and John Murkin contributed to the acquisition of data and drafting the article. PJ Devereaux contributed to the conception and design of the study, analysis and interpretation of data, and drafting the article.
Disclosures
None.
Funding statement
Hamilton Regional Medical Associates Resident Research Award.
Editorial responsibility
This submission was handled by Dr. Philip M. Jones, Associate Editor, Canadian Journal of Anesthesia.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Spence, J., Lamy, A., Bosch, J. et al. Feasibility of studying the association between intraoperative regional cerebral oxygen saturation and postoperative functional decline (ReFUNCTION): a pilot sub-study of NeuroVISION-Cardiac Surgery. Can J Anesth/J Can Anesth 67, 1497–1506 (2020). https://doi.org/10.1007/s12630-020-01777-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12630-020-01777-3