Warnings about an impending post-antibiotic apocalypse have, over the last five years, grown increasingly stark, with estimates placing the annual number of mortalities from antibiotic-resistant bacterial infections at 700,000 worldwide, a number that could rise to 10m in the next three decades.
The need for new classes of antibiotics has repeatedly been emphasised, with researchers turning to some of the most extreme environments on Earth in the hunt for new molecules. But finding broad-spectrum antibiotics that work against all classes of bacteria is challenging – and even if we discover new narrow-spectrum ones that work against particular strains, the likelihood of them becoming clinically available is slim. The economic realities of drug development mean that narrow-spectrum antibiotics aren’t cost-effective for pharmaceutical companies to produce.
“A lot of people say that the way forward is to improve the diagnostics and have a lot of narrow-spectrum antibiotics,” says Floyd Romesberg, a chemical biologist at the Scripps Research Institute in San Diego. “But, as things stand, that will never happen. Antibiotics are cheaply priced and don’t generate many sales because people only need them for a few days. Given how expensive they are to produce, pharma companies already struggle to make a profit on broad-spectrum antibiotics. So a narrow-spectrum antibiotic, which they’re going to sell even less of, just isn’t viable.”
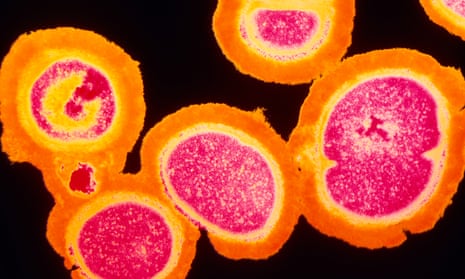
So, instead of searching for new compounds, many scientists are pinning their hopes on “superantibiotics”, essentially re-engineering existing drugs to overcome microbial resistance and make them thousands of times more potent. One of the problems with many antibiotics is that they need to get inside the bacteria cell to bind to it and kill it. And it only takes a single genetic mutation for a bacteria strain to render the antibiotic useless. So scientists have been exploring ways of changing the inherent killing mechanism and making it more lethal.
At Boston University, a team of biomedical engineers found that conventional antibiotics could kill between 10 and 1,000 times as many bacteria, including many previously resistant strains, when boosted with silver ions. This ancient remedy for infection – described by the Greeks in 400BC – works in two ways: first by disrupting bacterial metabolism, causing bacteria to self-destruct; and second by making their cell membranes more permeable to the antibiotic. However, while the research is promising, these drugs still have to pass safety testing, as ingesting too much silver can be toxic for humans.
A different approach, being explored at University College London (UCL), is creating a different killing mechanism by adding chemicals to a given antibiotic. This causes it to aggregate in clusters on the bacterial cell surface. These clusters dig into the bacteria and generate mechanical forces up to 11,000 times greater than those of conventional antibiotics – so strong that they can tear holes in bacteria, ripping them apart.
“So far, our work is at a very preliminary stage and we have still got to go through further preclinical [tests] and then clinical testing. But these kind of brute-force concepts circumvent many of the strategies bacteria have evolved to evade antibiotics,” says Joseph Ndieyira, a researcher at UCL. “This new mechanism is so lethal that they don’t have any defence to it.”
Such is the speed at which bacteria can adapt and evolve, that even when they re-engineer existing antibiotics, scientists face a challenge to get a drug that will last for decades, rather than a few years. During the past 50 years, we have already redesigned some of the earliest antibiotics, such as penicillin and fluoroquinolones several times. But we are now on to the fourth generation of penicillins, and newly resistant bacterial strains are never far away. “These drugs are more fragile because even the newer versions are still based on binding to different combinations of enzymes,” says Dale Boger, a chemical biologist at the Scripps Research Institute.
Instead, scientists believe durability can be achieved either by a killing mechanism, or by creating antibiotics with so many different killing mechanisms that the probability of bacteria developing a mutation is much lower. First developed in 1958, vancomycin is one of the so-called “last resort” antibiotics, reserved for the most dangerous infections where virtually nothing else will work. But during the past two decades, the rise of vancomycin-resistant bacteria has caused increasing consternation, prompting Boger and scientists at the Scripps Institute to attempt to create a super-form of vancomycin by engineering three new killing mechanisms into the original drug.
The result of their work, published earlier this year, is vancomycin 3.0, a drug that is 25,000 times more potent than before against previously resistant bacteria. The challenge is now to transform this elaborate molecule into something that can be made cheaply and on a vast scale. But Boger believes it may have the potential to last the test of time. “It’s hard to imagine a bacterium simultaneously making changes that could overcome three different mechanisms,” he says. “So the durability should be extremely high.”
One of the advantages of using vancomycin as the basis for creating a more durable antibiotic was that the original drug was already fairly robust. After 60 years, bacteria had only evolved one method of resistance. Boger believes the way forward is to take other robust antibiotics and add in mechanisms that make them even stronger. “There are great candidates to develop and re-engineer, and then you’d have a whole line of new drugs for which resistance would be very difficult to emerge.”
Comments (…)
Sign in or create your Guardian account to join the discussion