Abstract
Introduction
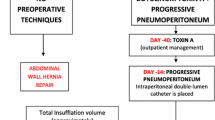
Incisional hernia with loss of domain (IHLD) remains a surgical challenge. Its management requires complex approaches including specific preoperative and intra-operative techniques. This study focuses on the interest of adding preoperative botulinum toxin A (BTA) injection to preoperative progressive pneumoperitoneum (PPP), compared to PPP alone.
Material
Patients between January 2015 and March 2020 with IHLD who underwent pre-operative preparation were included. Their baseline characteristics were retrospectively analyzed, along with the characteristics of their incisional hernia before and after preparation including CT-scan volumetry. Intra-operative data, early post-operative outcomes, surgical site occurrences (SSOs) including surgical site infection (SSI) were recorded.
Results
Four hundred and fifty (450) patients with incisional hernia were operated, including 41 patients (9.1%) with IHLD, 13 of which had both BTA and PPP, while 28 had PPP only. Both groups were comparable in term of patients and IHLD characteristics. Median increase in the volume of the abdominal cavity (VAbC) was + 55% for the entire population (+ 58.3% for the BTA-PPP group, p < 0.0001 and + 52.8% for the PPP-alone group, p < 0.0001) although the increase in volume was not different between the two groups (p = 0.99). Complete fascial closure was achieved in all patients. SSOs were more frequent in the PPP-alone group than in the BTA-PPP group (17 (60.7%) versus 3 (23.1%) patients, respectively, p = 0.043).
Conclusion
BTA and PPP are both useful in pre-operative preparation for IHLD. Combining both significantly increases the volume of abdominal cavity but associating BTA to PPP does not add any volumetric benefit but may decrease the post-operative SSO rate.


Similar content being viewed by others
Availability of data and materials
All data, materials and software application comply with field standards.
References
Fink C, Baumann P, Wente MN et al (2014) Incisional hernia rate 3 years after midline laparotomy. Br J Surg 101:51–54. https://doi.org/10.1002/bjs.9364
Lavanchy JL, Buff SE, Kohler A et al (2019) Long-term results of laparoscopic versus open intraperitonealonlay mesh incisional hernia repair: a propensity score-matched analysis. SurgEndosc 33:225–233. https://doi.org/10.1007/s00464-018-6298-6
Bosanquet DC, Ansell J, Abdelrahman T et al (2015) Systematic review and meta-regression of factors affecting midline incisional Hernia rates: analysis of 14,618 patients. PLoS ONE 10:e0138745. https://doi.org/10.1371/journal.pone.0138745
Kanitra JJ, Hess AL, Haan PS et al (2019) Hernia recurrence and infection rate in elective complex abdominal wall repair using biologic mesh. BMC Surg. https://doi.org/10.1186/s12893-019-0640-3
Kokotovic D, Bisgaard T, Helgstrand F (2016) Long-term recurrence and complications associated with elective incisional Hernia repair. JAMA 316:1575–1582. https://doi.org/10.1001/jama.2016.15217
Christoffersen MW, Helgstrand F, Rosenberg J et al (2013) Lower reoperation rate for recurrence after mesh versus sutured elective repair in small umbilical and epigastric hernias. a nationwide register study. World J Surg 37:2548–2552. https://doi.org/10.1007/s00268-013-2160-0
Slater NJ, Montgomery A, Berrevoet F et al (2014) Criteria for definition of a complex abdominal wall hernia. Hernia 18:7–17. https://doi.org/10.1007/s10029-013-1168-6
Passot G, Villeneuve L, Sabbagh C et al (2016) Definition of giant ventral hernias: development of standardization through a practice survey. Int J Surg 28:136–140. https://doi.org/10.1016/j.ijsu.2016.01.097
Lipman J, Medalie D, Rosen MJ (2008) Staged repair of massive incisional hernias with loss of abdominal domain: a novel approach. Am J Surg 195:84–88. https://doi.org/10.1016/j.amjsurg.2007.02.017
Eriksson A, Rosenberg J, Bisgaard T (2014) Surgical treatment for giant incisional hernia: a qualitative systematic review. Hernia 18:31–38. https://doi.org/10.1007/s10029-013-1066-y
Oliver-Allen HS, Hunter C, Lee GK (2015) Abdominal compartment syndrome as a rare complication following component separation repair: case report and review of the literature. Hernia 19:293–299. https://doi.org/10.1007/s10029-015-1362-9
Mavrodin CI, Pariza G, Ion D, Antoniac VI (2013) Abdominal compartment syndrome—a major complication of large incisional hernia surgery. Chirurgia (Bucur) 108:414–417
Angelici AM, Perotti B, Dezzi C et al (2016) Measurement of intra-abdominal pressure in large incisional hernia repair to prevent abdominal compartmental syndrome. G Chir 37:31–36
The Pediatric Guidelines Sub-Committee for the World Society of the Abdominal Compartment Syndrome, Kirkpatrick AW, Roberts DJ et al (2013) Intra-abdominal hypertension and the abdominal compartment syndrome: updated consensus definitions and clinical practice guidelines from the World Society of the Abdominal Compartment Syndrome. Intensive Care Med 39:1190–1206. https://doi.org/10.1007/s00134-013-2906-z
Renard Y, Lardière-Deguelte S, de Mestier L et al (2016) Management of large incisional hernias with loss of domain: a prospective series of patients prepared by progressive preoperative pneumoperitoneum. Surgery 160:426–435. https://doi.org/10.1016/j.surg.2016.03.033
Ramirez OM, Ruas E, Dellon AL (1990) “Components separation” method for closure of abdominal-wall defects: an anatomic and clinical study. PlastReconstrSurg 86:519–526. https://doi.org/10.1097/00006534-199009000-00023
Ramirez OM (2006) Inception and evolution of the components separation technique: personal recollections. ClinPlastSurg 33(241–246):vi. https://doi.org/10.1016/j.cps.2005.12.011
Carbonell AM, Cobb WS, Chen SM (2008) Posterior components separation during retromuscular hernia repair. Hernia 12:359–362. https://doi.org/10.1007/s10029-008-0356-2
Novitsky YW, Elliott HL, Orenstein SB, Rosen MJ (2012) Transversusabdominis muscle release: a novel approach to posterior component separation during complex abdominal wall reconstruction. Am J Surg 204:709–716. https://doi.org/10.1016/j.amjsurg.2012.02.008
Blair LJ, Ross SW, Huntington CR et al (2015) Computed tomographic measurements predict component separation in ventral hernia repair. J Surg Res. https://doi.org/10.1016/j.jss.2015.06.033
Zolin SJ, Fafaj A, Krpata DM (2020) Transversusabdominis release (TAR): what are the real indications and where is the limit? Hernia 24:333–340. https://doi.org/10.1007/s10029-020-02150-5
Hodgkinson JD, Leo CA, Maeda Y et al (2018) A meta-analysis comparing open anterior component separation with posterior component separation and transversusabdominis release in the repair of midline ventral hernias. Hernia 22:617–626. https://doi.org/10.1007/s10029-018-1757-5
Petro CC, Raigani S, Fayezizadeh M et al (2015) Permissible intraabdominal hypertension following complex abdominal wall reconstruction. PlastReconstrSurg 136:868–881. https://doi.org/10.1097/PRS.0000000000001621
Hadad I, Small W, Dumanian GA (2009) Repair of massive ventral hernias with the separation of parts technique: reversal of the “lost domain.” Am Surg 75:301–306
Qaja E, Le C, Benedicto R (2017) Repair of giant inguinoscrotal hernia with loss of domain. J Surg Case Rep. https://doi.org/10.1093/jscr/rjx221
Benoit O, Moszkowicz D, Milot L et al (2020) Right colectomy with absorbable mesh repair as a salvage solution for the management of giant incisional hernia with loss of domain: results of a bicentric study. World J Surg 44:1762–1770. https://doi.org/10.1007/s00268-020-05395-4
Alam NN, Narang SK, Pathak S et al (2016) Methods of abdominal wall expansion for repair of incisional herniae: a systematic review. Hernia 20:191–199. https://doi.org/10.1007/s10029-016-1463-0
Goñi Moreno I (1971) Pneumoperitoneum applied to the surgical preparation of large chronic eventrations. Prensa Med Argent 58:1037–1041
Moreno IG (1947) Chronic eventrations and large hernias; preoperative treatment by progressive pneumoperitomeum; original procedure. Surgery 22:945–953
Dumont F, Fuks D, Verhaeghe P et al (2009) Progressive pneumoperitoneum increases the length of abdominal muscles. Hernia 13:183–187. https://doi.org/10.1007/s10029-008-0436-3
LópezSanclemente MC, Robres J, López Cano M et al (2013) Progressive preoperative pneumoperitoneum in patients with giant hernias of the abdominal wall. Cir Esp 91:444–449. https://doi.org/10.1016/j.ciresp.2012.08.004
Ibarra-Hurtado TR, Nuño-Guzmán CM, Echeagaray-Herrera JE et al (2009) Use of botulinum toxin type a before abdominal wall hernia reconstruction. World J Surg 33:2553–2556. https://doi.org/10.1007/s00268-009-0203-3
Ibarra-Hurtado TR, Nuño-Guzmán CM, Miranda-Díaz AG et al (2014) Effect of botulinum toxin type A in lateral abdominal wall muscles thickness and length of patients with midline incisional hernia secondary to open abdomen management. Hernia 18:647–652. https://doi.org/10.1007/s10029-014-1280-2
Bueno-Lledó J, TorregrosaGallud A, Jiménez Rosellón R et al (2017) Preoperative preparation of loss of domain hernia. Progressive pneumoperitoneum and botulinum toxin type A. Cir Esp 95:245–253. https://doi.org/10.1016/j.ciresp.2017.04.006
Rodriguez-Acevedo O, Elstner KE, Jacombs ASW et al (2018) Preoperative Botulinum toxin A enabling defect closure and laparoscopic repair of complex ventral hernia. SurgEndosc 32:831–839. https://doi.org/10.1007/s00464-017-5750-3
Farooque F, Jacombs ASW, Roussos E et al (2016) Preoperative abdominal muscle elongation with botulinum toxin A for complex incisional ventral hernia repair. ANZ J Surg 86:79–83. https://doi.org/10.1111/ans.13258
Catalán-Garza V, Peña-Soria MJ, Sáez-Carlin P et al (2020) Long-term results of botulinum toxin type A in complex abdominal wall repair and review of the literature. Updates Surg. https://doi.org/10.1007/s13304-020-00775-w
Bueno-Lledó J, Torregrosa A, Jiménez R, Pastor PG (2018) Preoperative combination of progressive pneumoperitoneum and botulinum toxin type A in patients with loss of domain hernia. SurgEndosc 32:3599–3608. https://doi.org/10.1007/s00464-018-6089-0
Yurtkap Y, van Rooijen MMJ, Roels S et al (2020) Implementing preoperative Botulinum toxin A and progressive pneumoperitoneum through the use of an algorithm in giant ventral hernia repair. Hernia. https://doi.org/10.1007/s10029-020-02226-2
Elstner KE, Read JW, Rodriguez-Acevedo O et al (2017) Preoperative progressive pneumoperitoneum complementing chemical component relaxation in complex ventral hernia repair. SurgEndosc 31:1914–1922. https://doi.org/10.1007/s00464-016-5194-1
Bueno-Lledó J, Carreño-Saenz O, Torregrosa-Gallud A, Pous-Serrano S (2020) Preoperative botulinum toxin and progressive pneumoperitoneum in loss of domain hernias-our first 100 cases. Front Surg 7:3. https://doi.org/10.3389/fsurg.2020.00003
Kanters AE, Krpata DM, Blatnik JA et al (2012) Modified hernia grading scale to stratify surgical site occurrence after open ventral hernia repairs. J Am CollSurg 215:787–793. https://doi.org/10.1016/j.jamcollsurg.2012.08.012
Docimo S, Spaniolas K, Svestka M et al (2019) Increased incidence of surgical site infection with a body mass index ≥ 35 kg/m2 following abdominal wall reconstruction with open component separation. SurgEndosc 33:2503–2507. https://doi.org/10.1007/s00464-018-6538-9
Sabbagh C, Dumont F, Robert B et al (2011) Peritoneal volume is predictive of tension-free fascia closure of large incisional hernias with loss of domain: a prospective study. Hernia 15:559–565. https://doi.org/10.1007/s10029-011-0832-y
Stoppa R, Ralaimiaramanana F, Henry X, Verhaeghe P (1999) Evolution of large ventral incisional hernia repair. The French contribution to a difficult problem. Hernia 3:1–3. https://doi.org/10.1007/BF01576729
Kingsnorth A (2006) The management of incisional Hernia. Ann R CollSurgEngl 88:252–260. https://doi.org/10.1308/003588406X106324
Chevrel JP, Rath AM (2000) Classification of incisional hernias of the abdominal wall. Hernia 4:7–11. https://doi.org/10.1007/BF01230581
Parker SG, Halligan S, Liang MK et al (2020) Definitions for loss of domain: an international Delphi consensus of expert surgeons. World J Surg 44:1070–1078. https://doi.org/10.1007/s00268-019-05317-z
Parker SG, Halligan S, Blackburn S et al (2019) What exactly is meant by “loss of domain” for ventral hernia? Systematic review of definitions. World J Surg 43:396–404. https://doi.org/10.1007/s00268-018-4783-7
Mancini A, Mougin N, Venchiarutti V et al (2020) Goni Moreno progressive preoperative pneumoperitoneum for giant hernias: a monocentric retrospective study of 162 patients. Hernia 24:545–550. https://doi.org/10.1007/s10029-019-02113-5
Agnew SP, Small W, Wang E et al (2010) Prospective measurements of intra-abdominal volume and pulmonary function after repair of massive ventral hernias with the components separation technique. Ann Surg 251:981–988. https://doi.org/10.1097/SLA.0b013e3181d7707b
De Santis L, Frigo F, Bruttocao A, Terranova O (2003) Pathophysiology of giant incisional hernias with loss of abdominal wall substance. Acta Biomed 74(Suppl 2):34–37
Henriksen NA, Montgomery A, Kaufmann R et al (2020) Guidelines for treatment of umbilical and epigastric hernias from the European Hernia Society and Americas Hernia Society. Br J Surg 107:171–190. https://doi.org/10.1002/bjs.11489
Parker SG, Wood CPJ, Butterworth JW et al (2018) A systematic methodological review of reported perioperative variables, postoperative outcomes and hernia recurrence from randomised controlled trials of elective ventral hernia repair: clear definitions and standardised datasets are needed. Hernia 22:215–226. https://doi.org/10.1007/s10029-017-1718-4
Tanaka EY, Yoo JH, Rodrigues AJ et al (2010) A computerized tomography scan method for calculating the hernia sac and abdominal cavity volume in complex large incisional hernia with loss of domain. Hernia 14:63–69. https://doi.org/10.1007/s10029-009-0560-8
Kingsnorth AN, Sivarajasingham N, Wong S, Butler M (2004) Open mesh repair of incisional hernias with significant loss of domain. Ann R CollSurgEngl 86:363–366. https://doi.org/10.1308/147870804236
Punjani R, Shaikh I, Soni V (2015) Component separation technique: an effective way of treating large ventral hernia. Indian J Surg 77:1476–1479. https://doi.org/10.1007/s12262-015-1265-0
Novitsky YW, Fayezizadeh M, Majumder A et al (2016) Outcomes of posterior component separation with transversusabdominis muscle release and synthetic mesh sublay reinforcement. Ann Surg 264:226–232. https://doi.org/10.1097/SLA.0000000000001673
Cornette B, De Bacquer D, Berrevoet F (2018) Component separation technique for giant incisional hernia: a systematic review. Am J Surg 215:719–726. https://doi.org/10.1016/j.amjsurg.2017.07.032
Appleton ND, Anderson KD, Hancock K et al (2017) Initial UK experience with transversusabdominis muscle release for posterior components separation in abdominal wall reconstruction of large or complex ventral hernias: a combined approach by general and plastic surgeons. Ann R CollSurgEngl 99:265–270. https://doi.org/10.1308/rcsann.2016.0241
Fayezizadeh M, Majumder A, Belyansky I, Novitsky YW (2016) Outcomes of retromuscular porcine biologic mesh repairs using transversusabdominis release reconstruction. J Am CollSurg 223:461–468. https://doi.org/10.1016/j.jamcollsurg.2016.06.008
Jones CM, Winder JS, Potochny JD, Pauli EM (2016) Posterior component separation with transversusabdominis release: technique, utility, and outcomes in complex abdominal wall reconstruction. PlastReconstrSurg 137:636–646. https://doi.org/10.1097/01.prs.0000475778.45783.e2
Loh CYY, Nizamoglu M, Shanmugakrishnan RR et al (2018) Comparing transversusabdominus release and anterior component separation techniques in reconstructing midline hernias: a cadaveric study. J PlastReconstrAesthetSurg. https://doi.org/10.1016/j.bjps.2018.06.005
Pauli EM, Rosen MJ (2013) Open ventral hernia repair with component separation. SurgClin North Am 93:1111–1133. https://doi.org/10.1016/j.suc.2013.06.010
Torregrosa-Gallud A, Sancho Muriel J, Bueno-Lledó J et al (2017) Modified components separation technique: experience treating large, complex ventral hernias at a University Hospital. Hernia 21:601–608. https://doi.org/10.1007/s10029-017-1619-6
Winder JS, Behar BJ, Juza RM et al (2016) Transversusabdominis release for abdominal wall reconstruction: early experience with a novel technique. J Am CollSurg 223:271–278. https://doi.org/10.1016/j.jamcollsurg.2016.04.012
Blair LJ, Ross SW, Huntington CR et al (2015) Computed tomographic measurements predict component separation in ventral hernia repair. J Surg Res 199:420–427. https://doi.org/10.1016/j.jss.2015.06.033
Majumder A, Martin-Del-Campo LA, Miller HJ et al (2020) Evaluation of anterior versus posterior component separation for hernia repair in a cadaveric model. SurgEndosc 34:2682–2689. https://doi.org/10.1007/s00464-019-07046-9
Maloney SR, Schlosser KA, Prasad T et al (2019) Twelve years of component separation technique in abdominal wall reconstruction. Surgery 166:435–444. https://doi.org/10.1016/j.surg.2019.05.043
Ennis LS, Young JS, Gampper TJ, Drake DB (2003) The “open-book” variation of component separation for repair of massive midline abdominal wall hernia. Am Surg 69:733–742 (discussion 742–743)
Wegdam JA, Thoolen JMM, Nienhuijs SW et al (2019) Systematic review of transversusabdominis release in complex abdominal wall reconstruction. Hernia 23:5–15. https://doi.org/10.1007/s10029-018-1870-5
Lardière-Deguelte S, Appere F, Goia A-V et al (2010) Efficacité du pneumopéritoineprogressifpré- opératoiredans le traitement des grandeséventrations: évaluationvolumétrique par tomodensitométrie. E-mémoires de l’AcadémieNationale de Chirurgie 9:103–106. https://doi.org/10.14607/emem.2010.2.103
Martínez-Hoed J, Bonafe-Diana S, Bueno-Lledó J (2020) A systematic review of the use of progressive preoperative pneumoperitoneum since its inception. Hernia. https://doi.org/10.1007/s10029-020-02247-x
Weissler JM, Lanni MA, Tecce MG et al (2017) Chemical component separation: a systematic review and meta-analysis of botulinum toxin for management of ventral hernia. J PlastSurg Hand Surg 51:366–374. https://doi.org/10.1080/2000656X.2017.1285783
Bueno-Lledó J, Martinez-Hoed J, Torregrosa-Gallud A et al (2020) Botulinum toxin to avoid component separation in midline large hernias. Surgery. https://doi.org/10.1016/j.surg.2020.04.050
Cakmak M, Caglayan F, Somuncu S et al (2006) Effect of paralysis of the abdominal wall muscles by botulinum A toxin to intraabdominal pressure: an experimental study. J PediatrSurg 41:821–825. https://doi.org/10.1016/j.jpedsurg.2005.12.023
Funding
The present research did not receive any financial rewards.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Ahmad Tashkandi, Jules Durtette-Guzylack, Antoine Cayeux and Yohann Renard. The first draft of the manuscript was written by Ahmad Tashkandi and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
The present study includes patients operated on using routine and local standards. The two techniques reported in the present article were locally protocolized for a long time and followed the current state-of-the-science of incisional hernia management.
Consent for publication
Informed consent was obtained from all individual participants included in the study.
Consent to participate
The folders of all patients were retrospectively analyzed. All patients received adequate information and gave their written informed consent to be operated on following our local protocol.
Conflicts of interest
All authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Tashkandi, A., Bueno-Lledó, J., Durtette-Guzylack, J. et al. Adjunct botox to preoperative progressive pneumoperitoneum for incisional hernia with loss of domain: no additional effect but may improve outcomes. Hernia 25, 1507–1517 (2021). https://doi.org/10.1007/s10029-021-02387-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-021-02387-8