Over the past three and half years, I’ve had 70 wasp stings injected into my left arm. Voluntarily. This hasn’t been an exercise in masochism, but rather to ensure I can go outside without screaming from fear.
Every year in the UK, there are between two and nine deaths from anaphylaxis caused by bee and wasp venom. In 2015-16, there were 4,451 hospital admissions for anaphylactic shock. In an effort to avoid adding to these statistics again, I’ve completed an immunotherapy programme. Fingers crossed “the cure” is never put to the test.
On the day Andy Murray first won Wimbledon, I was celebrating with a run around the garden when I inadvertently stumbled upon a wasps’ nest. Unsurprisingly, the 1,000 inhabitants did not take kindly to me destroying their home. My joy at Andy’s victory turned to panic; instinctively, I waved my arms wildly, while an army of angry stingers pursued me around an apple tree, back into my house and into the shower. It would have looked amusing to any onlookers, but an hour later I was in A&E, my puffed-up body and dizzy mind showing the early signs of anaphylactic shock.
I recovered well, but for the next six months I was so scared of wasps that I hardly ventured outside, especially if ketchup or jam sandwiches were on display. And I love ketchup, and jam sandwiches.
My GP suggested that I do an immunotherapy course, which required a three-year commitment and regular appointments at Guy’s hospital in London. A programme of wasp venom injections was designed to build up my tolerance and eradicate my fear in case of a future wasp attack. After each injection I would be observed for an hour, to ensure I didn’t have an adverse reaction, before being allowed home.
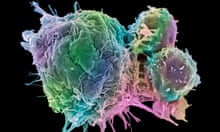
Immunotherapy works by gradually changing the immune system and educating cells not to overreact to venom. However, this process takes a long time to achieve, because it’s not just about immediate tolerance but permanent protection. Doctors have found three years is the optimum time for this long-term resistance to evolve.
First, there is an initial up-dosing phase, which involves weekly visits to an allergy clinic for up to three months. The amount of injected venom is gradually increased each time as this minimises the chances of any reaction. Appointments are then reduced to around every six weeks for the maintenance phase and injections increased to the equivalent of two and half wasp stings each session. Apart from a sore arm and a moderate amount of trepidation, I walked away unscathed.
Allergy UK’s head of clinical services, Amena Warner, says: “The criteria for being accepted for wasp immunotherapy is to have a previous anaphylactic reaction to wasps and a referral from a GP. The course is administered by subcutaneous injection. If someone can tolerate the dose in a clinical surrounding, then in all likelihood, if they are stung outside, they should be able to tolerate that as well. The best part is there is a 90% efficacy, which is very high. That is as near to a cure as we can possibly get.”
However, she adds: “Not all patients want to go through this type of treatment. The time commitment alone is very labour intensive and not everyone has the time.”
However, immunotherapy is now widely accepted as a way of dealing with many allergies that can’t be controlled by over-the-counter medication or prescriptions from the GP. And for the needle phobic, thankfully other allergies can be treated less intrusively. Allergies to cats, dogs, horses and pollen can be dealt with sublingually – by placing drops under the tongue. This can be extremely useful for patients struggling with occupational therapies, such as a vet who is allergic to cats, or a policeman susceptible to asthma attacks while raiding homes with animals.
For me, the alternative was to spend the rest of my life carrying an auto-injector filled with adrenaline and to remain constantly on high alert, especially during the summer months. If I was stung again, I’d have to jab myself in the thigh and hightail it to hospital. And although I was prepared to take the necessary precautions – always wear shoes, cover my food, never drink from a can – psychologically I didn’t want to be always wondering “what if”.
So, despite the long-term commitment required, I was happy to persevere, although it must be said, I was exceptionally grateful when it came to an end. Opinion is divided over whether it’s necessary to still carry an auto-injector after completing the course: some doctors believe it’s a necessary precaution, others say you are considered no more at risk than anyone else, and as a first line of action if ever stung again you should take an anti-histamine tablet. It’s all based on risk assessment.
As of yet, in the UK we don’t test the results at the end of the immunotherapy course in the same way as other countries. Warner says: “In some places a patient places their hand in box of wasps, waits to be stung and the reaction is checked. We wait for patients to tell us if they got stung.”








Comments (…)
Sign in or create your Guardian account to join the discussion