
Breast cancer today
Breast cancer is the most common cancer in the UK. Although it mainly affects women, it can also be developed by men. According to the World Health Organization, over half a million women died due to breast cancer in 2012 (Global Health Estimates, WHO 2013).
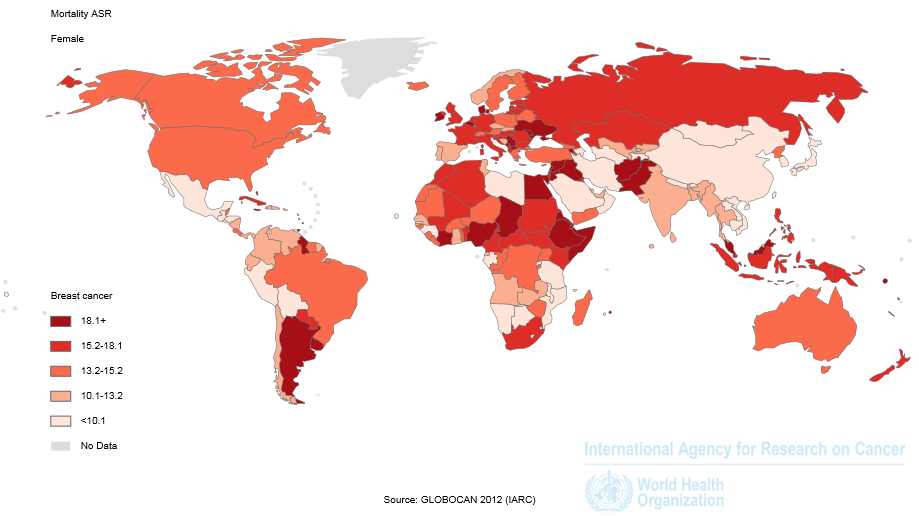
Image: World breast cancer mortality in women by Ferlay J. and colleagues. GLOBOCAN 2012. Cancer Incidence and Mortality Worldwide. International Agency for Research on Cancer (IARC) 2013. Available from https://globocan.iarc.fr/Pages/Map.aspx#.
Although the number of deaths remain high, due to successful prevention programs and early detection in developed countries, survival rates in the last decades have greatly improved. Today, early detection of breast cancer, increases the chances of successful management and cure of the disease. Approximately 90% of deaths due to breast cancer are linked to a late stage diagnosis, stages III and IV (read more about the stages here), and the spreading of the disease to other vital organs of the body (metastasis), which is why current efforts in the scientific community are directed towards preventing this step occurring. The articles highlighted below cover the latest lab-research aiming to improve personalized patient treatment, to the most recent improvements in the clinical practice of advanced breast cancer.
Towards personalized medicine
Although we generally refer to breast cancer as one disease, there are multiple subtypes of breast cancer that require different treatments. During the past decade it has become increasingly clear that in each patient, tumors evolve in a distinctive, unique way, which has led to the conclusion that individualized or personalized therapies are key in the treatment of the advanced stage of the disease.
New technique facilitates therapy personalization
Personalizing a therapy consists of studying the unique cellular and molecular composition of a patient’s tumor and then subsequently designing an optimal treatment for this person accordingly. The only problem with these therapies is that they are difficult to implement in practice because they are time consuming and very expensive for health care systems. Therefore, it’s important to find new techniques that will allow testing of multiple drugs in patient’s tumors. In an article published in BMC Cancer this year, the authors describe a new method for testing different drug combinations in the tumor of a patient after surgical removal. The researchers developed a way to maintain a living section of the patient’s breast tumor in a petri dish, which can then be tested with various treatments to find the optimal therapy for each patient. This method is particularly relevant as it can avoid treating patients with drugs that will not work for them, saving them time and the discomfort of unpleasant side effects.
Image of a patient’s tumour section by Naipal and colleagues. BMC Cancer. DOI: 10.1186/s12885-016-2119-2.
Improving clinical practice
After exploring new advances coming from the laboratory that promise a better future for breast cancer patients, now we will focus on how clinical practice is changing to offer improved breast cancer prevention and diagnosis.
Prevention: body weight remains a top risk factor in breast cancer
Prevention remains the most promising strategy for reducing breast cancer incidence and mortality. Research has identified the main risk factors associated with breast cancer occurrence, and the good news is that it is estimated that one third of the most common cancer types could be prevented by changes to the foods we eat and the amount of physical activity we do (World Cancer Research Fund – Continuous Update Project).
A new report published last month in BMC Cancer, corroborates evidence that being overweight and weight gain in general during adulthood is linked to an increased risk of breast cancer after menopause. The researchers conducted a large population study, including 739 cases of breast cancer compared to 815 healthy women. Weight variations were analyzed, including weight a year before diagnosis, in women of 20, 40 and 50 years of age. The data obtained indicated that postmenopausal cancer is associated with significant weight gain after the age of 40.
This study adds to the building evidence highlighting the importance of prevention in breast cancer incidence, and endorses more control over weight gain in middle age women.
Diagnosis: choosing the right imaging technique to achieve early diagnosis
Early diagnosis is the most effective way to reduce breast cancer mortality. Surgical removal of tumors complemented with adequate treatments has achieved a significant improvement in survival of early diagnosed breast cancer. The initial assessment of a potential breast cancer case is done using non-invasive imaging techniques that allow clinicians to see the inner tissue and find the tumor mass. There are currently multiple imaging techniques available, and the latest comparative analysis published in BMC Cancer aids clinicians when choosing the appropriate technique to increase diagnostic accuracy. Mammography is the gold standard technique for breast cancer diagnosis, being harmless and providing good results in most women. However, in women with denser and smaller-sized breasts the technique is not able to produce clear images for diagnosis. With this problem in mind, Yu and colleagues examined women diagnosed with breast cancer using gamma imaging, mammography, ultrasound and magnetic resonance before surgery. The analysis concluded that high resolution specific gamma imaging provides the sensitivity and specificity needed to diagnose women with dense or small breasts.
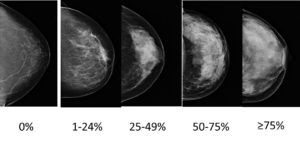
Images show mammograms of normal breasts of different densities – low to high from left to right. Credit: Caroline Diorio, Oncology Division, St Sacrement Hospital. Canada.
Although prevention can achieve a decrease in the incidence of breast cancer, these strategies cannot eradicate the majority of breast cancers that develop in low- and middle-income countries where breast cancer is diagnosed in very late stages. Therefore, early detection to improve breast cancer outcome and survival remains the keystone of breast cancer control, particularly in women with dense breasts where detection is more challenging, and in men, where a lack of public awareness remains.
The first question that might come to mind is: is this a thing? Indeed, male breast cancer is very rare. Compared to the 50,000 women diagnosed with breast cancer every year in the UK, only 350 men are affected, and therefore the condition is generally overlooked. To change this, in 2009 the male breast cancer advocacy groups Out of the Shadow of Pink, A Man’s Pink, and the Brandon Greening Foundation for Breast Cancer in Men joined together to globally establish the third week of October as “Male Breast Cancer Awareness Week”.
But males don’t have breasts, how can they develop breast cancer? Well, males do actually have a small amount of breast tissue under the nipples. Generally, due to the low levels of ‘female hormones’ this tissue remains inactive, however, a hormone imbalance at any point in life can cause the breast tissue to grow, and on occasion, uncontrolled growth can lead to breast cancer.
Image: MRB Priza. CC 2.0.
Given the low incidence of male breast cancer, it’s difficult to conduct research with a large number of patients to achieve conclusive evidence, and therefore treatment is generally adopted from female breast cancer guidelines. Recognizing the lack of public and clinical awareness about male cancer, we wanted to highlight one of the studies published in BMC Cancer adding further evidence to the current knowledge of breast cancer in men. The authors analyzed patient’s data including age, weight, risk factors, family history, tumor characteristics, treatment received and long term survival in all breast cancer patients attending their hospital over 15 years. In line with previous findings, the analysis revealed that those men having BRCA1/2 mutations, the most common mutation in hereditary breast cancers, display significant reduced survival. Among the risk factors, obesity and family history of breast cancer were associated with 21 % and 30 % of the cases respectively. Yet, a general positive message was conveyed, the study showed a high long-term survival rate in patients with male breast cancer compared with previous analyses. Given the low number of male breast cancer cases, reports like this one analyzing available patients’ data play a crucial role in shedding light into this rare condition.
A bright future ahead
Thanks to the advances achieved over the last decades in healthcare, today we live longer. With an increasingly ageing population worldwide, the incidence of Breast Cancer may also rise. As covered in this blog, evidence demonstrates that prevention and early diagnosis could help to eradicate this still deadly disease. Nevertheless, to achieve a world free of Breast Cancer deaths, public awareness about prevention programs and further research into the late stage of the disease is needed.
We hope that through exploring some of our recently published Breast Cancer Research, we have increased your awareness for breast cancer research and furthered your enthusiasm to support this cause.
Comments