In Type 1 diabetes, the body's immune system destroys the cells that produce insulin, leaving your body unable to make it. In Type 2 diabetes, the body continues to produce insulin, but organs don't respond to it efficiently. As a result, insulin injections, which effectively treat Type 1, don't do as much to help people with Type 2 diabetes.
There is a class of drugs called thiazolidinediones that help restore the body's ability to respond to insulin. Unfortunately, these drugs also cause a variety of side effects, including weight gain, bone density loss, and heart problems, so the search for a less problematic treatment has continued.
Now, working with mice, researchers have found that a well-known growth factor also restores the body's sensitivity to insulin and does so without any of the side effects associated with existing drugs. And they show that a modified form of the growth factor can still work effectively while reducing the risk of unforeseen consequences. This doesn't mean that using this method as a treatment will be free of side effects, but it does provide a promising avenue for further experiments.
The idea behind the new work came from reasoning about the existing drugs. Thiazolidinediones act by manipulating an existing signaling network called PPARγ; the side effects are thought to come from changes to this signaling network as well. So the authors started looking at changes that occur within this network, reasoning that if they could only activate a limited subset of it, they might be able to affect insulin signaling while limiting the side effects.
Recently, two different members of a family of signaling molecules called fibroblast growth factors (FGFs) were found to be activated by PPARγ signaling. One of them, FGF21, was found to lower blood glucose in rodents, but it also triggers the loss of bone density that existing drugs cause. The other is FGF1, which had already been implicated in insulin signaling, since mice where the gene was deleted develop diabetes when on a high-fat diet.
The authors test FGF1 injections in a number of mouse strains that have developed insulin-resistant diabetes. In all of them, a single injection restored insulin's ability to lower glucose levels. The response was dose dependent (the more you injected, the better the response) and could be maintained for up to 30 days of every-other-day injections, the longest period the authors tried. The initial FGF1 injection caused a temporary drop in the animals' food intake, but the effects on insulin were independent of that.
Diabetes and obesity are both associated with an inflammation of adipose tissue, so the authors looked at indications of inflammation. FGF1 injections reduced them. The longer treatments didn't seem to alter the animals' body weight or cause any obvious internal changes, and the animals showed none of the side effects associated with existing drugs.
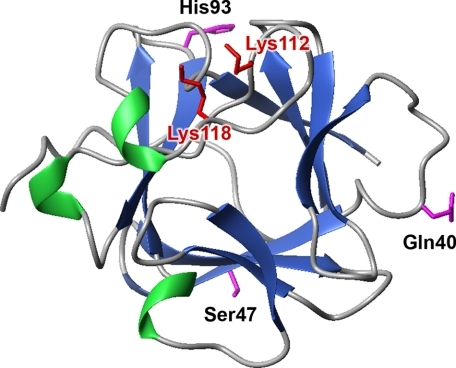
The one worry the authors had is that FGF1, as its name implies, is a growth factor, so it causes cells to divide. This raises the prospect that FGF1 treatment over the long term could ultimately result in an increased incidence of cancer. But FGF1 has been studied extensively, and other researchers had identified a shortened form that doesn't increase cell division. When tested on mice, this version was still able to effectively restore insulin sensitivity.
Clearly, longer-term studies are needed to get a better handle on potential side effects, and there's still the possibility that they'll miss something, given that mice aren't very good at explaining how they're feeling. The molecule itself tends to stick to any cell it comes into contact with (in fact, most cells use it to tell themselves and their neighbors to divide, since it rarely gets very far without sticking to something). This means it gets cleared from the blood supply very rapidly. It may also be possible to engineer a longer-lived form.
That, however, will probably wait until after more detailed searches for potential side effects.
Nature, 2014. DOI: 10.1038/nature13540 (About DOIs).
reader comments
70