The surgeon, who has spent 15 minutes gently tearing through tissue, suddenly pauses to gesture ever-so-slightly with his tiny scissors. "Do you see what's on this side? That's nerves." He moves the instrument a few millimeters to the right. "And on this one? That's cancer."
Ashutosh Tewari is the head of the urology department at Mount Sinai Hospital in New York City. He is in the process of removing a patient's cancerous prostate, the walnut-sized gland in the delicate area between the bladder and the penis. This surgery—one of three that Tewari performs on an average day—takes place entirely within an area the size of a cereal bowl. Tewari's movements are deliberate and exact. Just a few wrong cuts could make the patient incontinent or unable to perform sexually for the rest of his life.
But Tewari is making those cuts from 10 feet away. With a robot.
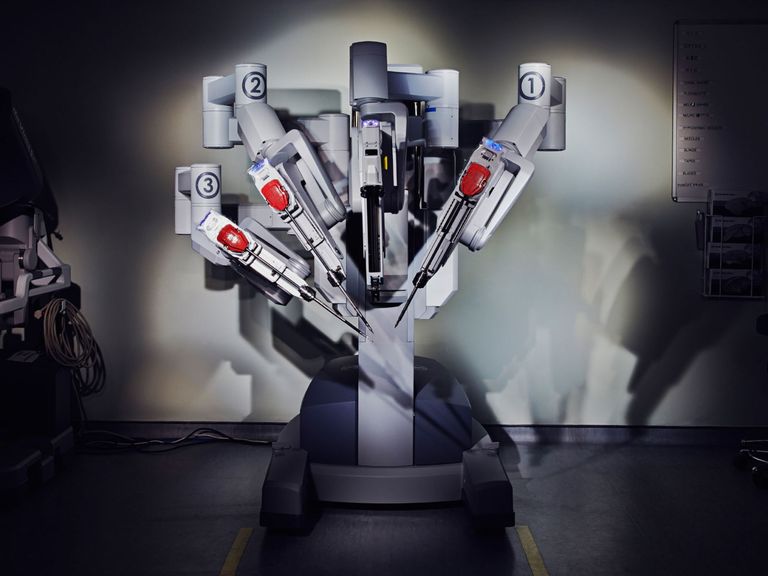
From where I'm standing in the operating room, the patient is partially obscured by the large multi-armed robot that looms over him, as well as the team of surgical assistants and anesthesiologists that surround him. Tewari, meanwhile, sits at a large console. He stares into the 3D display while manipulating levers with his hands and fingers, which give him some haptic feedback. While the system resembles an old-school arcade video game, Tewari insists that there's nothing game-like about it. Surgery is serious business.
Even from across the room, robots can make surgery better. For the surgeons, sitting at a console is less physically taxing than hunching over the body during an open procedure. The software is so sophisticated that it corrects a surgeon's shaking hand. The zoomed-in camera view takes some getting used to, but for working in a small area, it's great.
The real benefits, though, are for the patient. Thin, dexterous tools are precise over a large range of motion. For example, Tewari used the forceps to tie a series of knots with thin string to suture up his incisions, which makes it easier for surgeons to spare healthy tissue when cutting out an unwanted mass. Tewari says that at his hospital, the use of robots has cut the recovery time for prostate surgery from four days to just one or two. No surprise, then, that robotic procedures are more popular than ever. In 2010, 86 percent of prostatectomies were done with robots, and they are used to operate on hearts, kidneys, gallbladders, and ovaries. In 2012, 450,000 operations were done with robots, according to theWall Street Journal.
Here's the thing, though: Robot assistants are just the beginning. After all, if a surgeon can operate from across the room, then it follows that she could operate from across the world, as long as she has a strong internet connection. Remote robotic surgery—doctors using these robotic assistants to operate from miles away—seems to be the inevitable next step.
Scientists first demonstrated remote surgery in 2001, when a surgeon in New York operated a robot to remove a patient's gallbladder in France. Since then, surgeons from afar have operated robots in underwater bases and in remote Canadian hamlets. Combined with a team of healthcare professionals attending to the patient on the ground, the best surgeons in the world could stay close to home while performing operations on people in countries with limited medical infrastructure, or on astronauts in space, or on soldiers at the front lines of battle.
Yet even now, 15 years after their first real-world demonstration, remote surgical platforms aren't yet used outside of these experimental or extreme settings. Some optimistic experts says it's only a matter of time until researchers fix the technical challenges that prevent doctors from operating from another state or country. But from cyber security to connection speeds to legal gray areas, there are a host of potential problems with remote surgery. Under the wrong conditions or in the wrong hands, surgical tools can do more harm than good.
There Is a Lag
At its most basic, telesurgery is done the same way as all two-way communication on the Internet. The surgeon is on one end with a console that allows her to manipulate the robot. That information, transmitted in a coding language specific to surgical robots, is sent through the hospital's router and modem, then hops through a few servers until it reaches the modem and local router of its intended recipient. Then it tells the robot how to move. Cameras and haptic sensors bring feedback back to the surgeon through the same path. In more remote settings, the wireless signal might have to bounce off a satellite or flow through a router hovering over the surgical site on a drone.
If we have the technology and the expertise to conduct telesurgery, why isn't it happening for everyday procedures? One simple reason may be the sheer cost of the robot, says Grant Schaffner, president of ProtoStar Engineering who first became interested in using robotic surgery tools on astronauts. "The technology is there already, but either the cost needs to come down, or the end users need to find the financial resources to invest," he says. For a few elite hospitals like Mount Sinai, investing in those tools makes sense and can even be a draw for patients. But most hospitals—especially those in developing countries, where international medical expertise from afar would be most helpful—can't afford them. Even without the capability for telesurgery, surgical robot systems like the one Tewari used at Mount Sinai cost about $2 million each.
Even if remote clinics and hospitals could afford the machines, that is not enough. The digital infrastructure there may not even have enough bandwidth to transmit the enormous amount of data moving between surgeon and robot. Blake Hannaford, one of the creators of the RAVEN telesurgery robot, says that uncompressed video streaming requires a bandwidth of at least 2 megabits per second (that's less than it takes to stream a high-definition video from YouTube), and experts are not yet sure what kind of resolution is absolutely necessary. That's probably feasible in hospitals with fast private networks, but it might not work in rural places with limited digital infrastructure or shared networks.
But even under the most ideal circumstances, remote surgery has several issues caused simply by the distance between surgeon and patient. And so far, no one has quite been able to resolve them.
One of the biggest is lag time. In a robotic surgery where robot and surgeon are in the same room, wires connect the control console directly to the surgical robot. Used this way, the robot and console create a closed loop that leaves little room for signal delay. More distance between surgeon and patient means greater delay between action and command, and that can be bad news. If you're making the most delicate of surgical cuts, you want instant, perfect feedback and visuals.
Last year, a pair of researchers conducted an experiment to see just how much lag time would hamper a surgeon's performance. They had 20 surgeons complete four different tasks with a robotic surgery training tool. The device's software tracked their success, but it also added a randomized delay between 100 and 1,000 milliseconds. The researchers found that the surgeons didn't notice if the lag time was less than 250 milliseconds. Higher than that, though, and their performance suffered no matter their level of surgical experience
The delays are caused in part by physical distance, but mostly by obstacles in the digital networks. As information arrives in specific homes or businesses, it's funneled into fewer wires. It's further slowed as it's checked for viruses. These impediments act as "invisible barriers" slowing the relay between the two robotic tools, says Roger Smith, a robotic surgery researcher at the Nicholson Center in Orlando and one of the study authors.
For example, the signal arriving in Orlando from Denver, over 1,000 miles, was delayed up to 150 milliseconds—the same maximum delay as the data that came from Tampa, just 85 miles away. Though a real procedure would probably be conducted through a virtual private network (VPN), Smith adds, those invisible barriers—and not distance—would be the determining factor of whether a procedure is possible with 2,000 miles between patient and doctor, or just two miles.
The other big problem? Anything that is connected is also vulnerable.
Hacking Surgery
"As you separate surgeon from robot by distance and through a communication network, you open up the opportunity of hacking—that's why we decided to look at the security question," says Howard Chizeck, a professor of electrical engineering at the University of Washington.
To see just how vulnerable these tools really are, Chizeck and his team of electrical engineers and computer scientists decided to find all the different ways to hack a robotic surgery tool called the RAVEN II. For their study, published in April in the open-access journal arXiv, the researchers set up a surgeon (in this case a graduate student with a rudimentary understanding of the system) and a robot (used here to move blocks around a table, not to operate on a real person). Information moved between the two by passing through a central network hub, to which an "attacking machine" was also connected. As code moved between the surgeon and robot, the attacking machine tried to alter or interrupt the messages—a "man-in-the-middle" style of attack.
The researchers wrote special bits of code to delay information or to replace those given by the surgeon. No matter what they tried to attack—changing the position of the surgical tool, delaying the surgeon's command, forcing the system to reset—they succeeded. Many times, the "surgeon" didn't even notice that the system wasn't behaving as it should.
Malfunctioning surgical robots could be dangerous for patients even under the most mundane circumstances. As a hacker uses a surgical robot to gain entry to a hospital's confidential database or manipulates the tool's movements just because he can, the blade could make an extra incision and damage a nearby organ, or a patient could simply bleed out if a machine stops moving during an operation. "But in a battlefield situation, delayed or modified messages can turn a surgical tool against you," Chizeck says. "It turns into a weapon."
Bolstering the digital security for surgical robots may prove to be the biggest challenge. But it's more essential than ever, since hacks now seem inevitable. At least five health insurance companies were hacked last year, putting more than 100 million patients at risk. Afterward, a Washington Post headline called 2015 the "year of the healthcare hack."
Data encryption is the first logical step to protecting the communication between surgeon and robot, Chizeck and his colleagues write. Unlike smartphones or bank databases, surgical robots (like many other medical devices) don't encrypt their data when they transmit it, nor do they have sophisticated authentication procedures for users to log in, says Stephen Wu, an attorney at the Silicon Valley Law Group who specializes in information security. That leaves them more vulnerable to attack.
But even encryption wouldn't be a cure-all. Anything connected to the Internet could be hacked, and surgical robots are no exception. Manufacturers need to offer software updates to patch up shifting holes in devices' digital protection, which they are sometimes reluctant to do today. Hardware and software companies can also collaborate to make the devices more sensitive to infiltration thanks to more creative approaches to cybersecurity.
Take the idea of a "surgical signature," for example. Because every surgeon operates the controls a little differently, software could identify that unique pattern and use it as a security feature, just like a person's fingerprint. If the system doesn't recognize the signature all of a sudden, it would know somebody else has hacked in and could take pre-planned actions to stop the attack.
Of course, surgical tools can't just stop in the middle of a surgery—a patient could die if the robot just locked up or quit. Instead, surgical robots could have instructions to repeat a certain action. Say, if the system were hacked while a surgeon was stitching up a patient, the robot could simply keep doing that operation while the system alerts the doctors to the breach. It's not perfect, but it's better than simply stopping.
Chizeck and other experts say these kinds of security features must be worked into the robots' design. But so far, manufacturers are under no pressure to do so. "Ideally, [digital security] should start in the design phase of the product, at the beginning of the conceptualization. But that doesn't mean it always happens that way," Wu says. At the moment, telesurgery appears to have a chicken-and-egg problem. Because these procedures are still so rare, no hacking incidents have yet been reported, and the FDA doesn't require strict security provisions before a product goes to market. But the idea of surgery bots getting hacked is so nightmarish, the doctors say, that designers need to be worried about it now.
However, remote surgery seems to fall into a legal gray area. The FDA has approved the devices, but many doctors—including several interviewed for this piece—aren't clear on the regulations for the surgical procedures themselves, or the laws surrounding liability should the procedure go wrong. That's because many of those laws don't yet exist, says Bryant Walker Smith, a law and engineering professor at the University of South Carolina. It's a lot like the legal situation surrounding self-driving cars: regulatory bodies tend to implement rules only as issues come up. While that's fine for manufacturers hurrying to put surgical robots on the market, it also means that patients might be at higher risk when they go under the (robotic) knife.
Robot, M.D.
Surgeons who would operate from afar have reason to be optimistic. First, access to the necessary technology will likely improve. As more manufacturers rush to produce surgical robots—Google spinoff Verily just announced the creation of its surgical robot division, for example—the cost will drop, allowing more hospitals around the world to buy telesurgery tools. Connection speeds, too, will get better. Around the world, the Internet is getting faster every year, so finding quick enough connections for remote surgery will only become easier.
Minimizing lag time would require a few more experiments. If they know just how distance affects the delay between surgeon's command and robot's action, regulatory agencies could make sure telesurgical procedures take place within a particular distance. So far, however, experts don't yet know what that distance may be, especially when taking connection speeds into account.
Despite the barriers to making it more widespread, telesurgery wouldn't be too difficult to conduct with technology available today. But experts expect a whole new set of issues for what they assume to be the next iteration of mechanized surgical technology: Autonomous surgical robots.
Schaffner, when he was an aerospace engineering professor at the University of Cincinnati, was investigating telesurgery for astronauts when he realized that the lag time would be too long—more than two seconds—if the spacecraft was outside the Earth's atmosphere. He wondered: Could robots be trained to conduct procedures themselves?
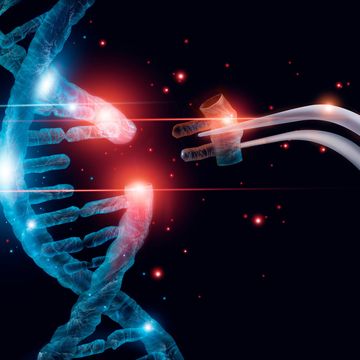
The idea isn't so ludicrous. In 2013, researchers created a robot that could autonomously remove patients' tissue for a biopsy. And so far Schaffner's team has made a lot of progress advancing procedures that are significantly more complex than that. In their setup, machine learning software picks up how surgeons manipulate the tools as the doctors "operate" on digital 3D scans of real patients. The robot can then mimic the surgeon when conducting the procedure on the actual patient. The artificial intelligence isn't quite sophisticated enough yet for the robots to do the procedures totally autonomously, Schaffner says: "People are squishy, organs move around a bit, and a robot needs to be smart enough to make adjustments on the fly." So for now a surgeon should be looped in to intervene should anything in the procedure not go as planned.
By summer 2016, Schaffner and his team hope to run their first real test by having a robot autonomously implant a hearing aid deep in a cadaver's ear. With more money into research and an accelerated approval process from the FDA, Schaffner could envision robots conducting biopsies, or even more sophisticated procedures like prostatectomies and appendectomies, in the next 10 to 20 years.
The Human Touch
Most experts agree that telesurgery could soon become commonplace. The early pioneers will likely run into some regulatory or technical snags, so doctors need to do their best to inform patients of the risks, as they would do with any procedure. And for most, the risks are not prohibitive. "There might be a small risk with some of these integrated medical procedures, but the benefit far outweighs them," says Dmitry Oleynikov, the chief of gastrointestinal and minimally invasive surgery, at the University of Nebraska Medical Center. "We just have to be thoughtful in how we apply these technologies. We need to make sure we aren't exposing patients to [unnecessary] risk."
Surgeons who using robots at close range today are usually more concerned about immediate threats to a patient's well being. Data breaches or abstract legal questions are often far from their minds. There can be issues with anesthetic, or a patient could have complications from a procedure, or he could simply slide off the table during an operation. While the robot makes a surgeons like Tewari's job easier and is better for the patient, it's merely a means to an end.
After the prostate surgery, Tewari exits the operating room and tells the patient's wife that the surgery went perfectly. She gives him an effusive hug. He tells me:
"From my standpoint, the patient has cancer, and [the robot] gives me an edge to removing it. I use the robot, which makes me a bit distant, but I'm still connected to my patients. It's human, and it's personal."
Want to know more about the future of surgery? Come talk to Alexandra Ossola on Digg on February 10 at 1 p.m. ET! It'll be more fun than having a robot remove your gallbladder.