Editor’s Note: Vital Signs is a monthly program bringing viewers health stories from around the world
Story highlights
Dengue fever is now endemic in more than 100 countries
Globally, there are more than 50 million infections each year
A bite from a single mosquito can result in fever, headaches, and pain. Severe cases can experience a multitude of symptoms including bleeding, shock, organ failure – and potentially death.
There is no treatment or vaccine and no real means of protecting yourself in countries endemic for the disease.
Though affected countries were once few, today more than 100 harbor the risk of infection – putting more than half the world’s population at risk and resulting in 50 million infections each year.
Read: This man’s blood saved 2 million babies
The infection is Dengue – formerly known as “break-bone fever” because of the severe joint points it causes – and it’s spread by one of nature’s toughest, most versatile mosquitoes – and it’s not the one that spreads malaria.
Coexisting with humans
“It lives, eats and breathes humans” says Duane Gubler, professor of Infectious Diseases at Duke University Medical School, Singapore. Gubler has been working on Dengue control for more than 45 years and founded the Dengue Branch of the U.S. Centers for Disease Control (CDC). He has witnessed the epidemic expanding globally – through the opportunistic mosquitoes harboring the disease.
“Urbanization provided the ideal ecology for these mosquitoes,” says Gubler, referring to the increased density of populations as people flock to cities in search of employment, bringing with them endless supplies of blood for pregnant mosquitoes that need to nourish their eggs.
Read: The worms that invade your brain
The villain carrying the Dengue virus is the Aedes mosquito and it comes in two forms: Aedes Aegyti and Aedes albopictus, with the former causing the greatest degree of infection. “They’ve become highly urbanized and highly adapted to humans,” says Gubler.
This species can also carry the virus behind other diseases such as Yellow fever, chikungunya and lymphatic filariasis. But Dengue is the disease that has spread most widely. Their success lies in their ability to bite during the day – unlike the mosquitoes harboring malaria – meaning they’re difficult to avoid.
“Using bed nets isn’t particularly useful for Dengue,” says Harold Margolis, current chief of the CDC’s Dengue branch. Bed nets have proven critical in the fight against malaria as the Anopheles species of the mosquito, which carries the malaria parasite, bites primarily at night.
Whilst people can cover up or resort to repellant, Margolis advises people in affected regions to simply tidy up. Any form of container in which shallow water can accumulate provides the perfect breeding ground for a female mosquito in search of a place to lay her eggs. “They can breed anywhere,” says Margolis – including the surface of trash cans, containers and used tires. “Anything that collects water will allow mosquitoes to reproduce in that water,” he says.
Easy breeders
Surface water, human blood and warm temperatures provide the perfect environment for these mosquitoes to flourish.
Read: Contact lens with built-in telescope
With no drug or vaccine yet available, the main form of disease prevention to date has been mosquito control – through the large-scale spraying of insecticides. The chemicals have been deployed in both residential and public spaces in a mass culling of the insects spreading the disease, taking other diseases carried by these mosquitoes with them. But the sprays haven’t been able to beat their versatile opponents – especially with humans further aiding the spread of infection.
“It’s people who move the infection around,” says Margolis.
Up to 75% of those infected never develop symptoms of Dengue, making it easy for the virus to be transported as people move around. When someone carrying the virus in their blood enters an area native for Aedes mosquitoes, they bring with them the potential to spread the disease. “Travelers come back with it and you get small outbreaks,” says Margolis.
In October 2012, an outbreak of Dengue occurred in Madeira, Portugal, resulting in 18 confirmed and more than 190 potential infections in a country where the disease is not normally found.
“Dengue is responsible for about 10% of people who come back from holiday with a temperature,” says Erik Sloan, an infectious disease clinician at the Liverpool School of Tropical Medicine, in the UK, who has seen a rise in the number of cases he’s treating. “We see more patients with Dengue than we did 10 or 20 years ago,” he says. The challenge for medics like Sloan is both diagnosing the disease, as many other infections cause fevers, and managing his patients when there is no treatment available.
Treating patients requires close monitoring in case the infection progresses to the more severe form of the disease, with symptoms such as internal bleeding and multiple organ failure. “Normally there’s a high chance you’ll be completely fine,” says Sloan. But he doesn’t get complacent. “If severe, there is a 12% risk of mortality,” he adds.
But despite its low mortality rate and ability to go unnoticed, Dengue has become a public health problem across the globe. Before 1960, only pockets of South America and south-east Asia were at risk of the disease, but now it is present across all continents.
Gubler blames it on international travel.
“What we’ve seen coincides perfectly with the advent of the jet airplane,” he says. The airplane is instrumental in transporting the virus – and the mosquito – to new populations with no immunity to the disease. “Three billion people will get on an airplane and travel somewhere in 2015,” he adds.
Air travel has also aided the movement of people towards urban centers and increased density in cities worldwide. More than half the world’s population currently live in cities and this figure is expected to reach 70% by 2050.
What can be done?
“Dengue is one of the diseases we haven’t been so successful in tackling or curbing,” says Dirk Engels, director of the Neglected Tropical Diseases department at the World Health Organization. “We don’t have easy tools to curb the spread of Dengue,” he says.
Engels hopes collaborations with pesticide producers could enable better designed programs to kill mosquitoes in the field. Another – more novel – strategy is the use of sterilized male mosquitoes to prevent future breeding.
“We’ve got to prevent transmission,” warns Gubler. In his eyes, the tools needed are mosquito control, drugs and a vaccine – the latter of which is now starting to show promise in terms of protection.
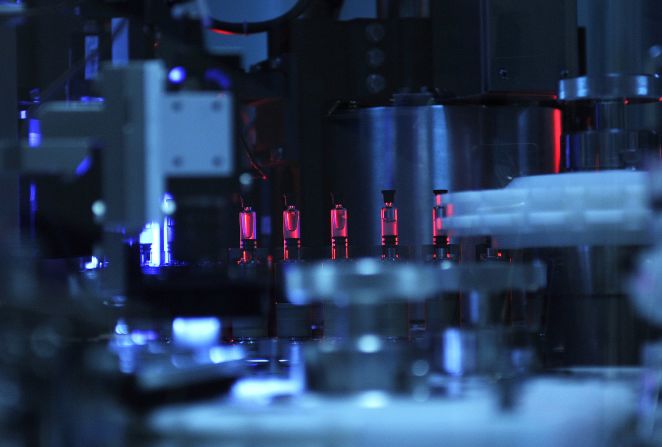
Six vaccines against Dengue have reached clinical trial stages to date and Gubler predicts three of the lead candidates will soon be licensed. Leading the way is pharmaceutical company Sanofi, whose vaccine was shown to cut incidence of the virus by 61% in late-stage trials.
This level of protection is enough to make a difference. “Even though it’s only partially effective, they’ll have public health utility,” says Gubler, who describes the search for a drug to treat the disease as a long road, with no trials for their efficacy reached just yet – but he’s hopeful.
“In the next three to five years we’ll see one or more antivirals come on as well,” he says.
With drugs and vaccines finally in the pipeline, the disease could be tackled head on – but not stopped completely.
“We’ll never eradicate it,” says Gubler. “But if we can use these new tools, we can control it as a public health problem.”